Introduction
Parkinson’s disease (PD) is a progressive neurodegenerative disorder affecting movement, often diagnosed through clinical evaluation. However, differentiating PD from other conditions with similar symptoms, known as Parkinsonism, can be challenging. In cases where diagnosis is unclear, Dopamine Transporter Scan (DaT Scan), a sophisticated imaging technique, becomes invaluable. This study investigates the impact of DaT Scan imaging on the diagnostic accuracy and subsequent clinical care for individuals presenting with Parkinsonism. While seemingly unrelated to automotive diagnostics tools like the Obd Scanner Et105, DaT scans represent a crucial diagnostic instrument in the medical field, offering precision akin to the detailed analysis provided by tools like the OBD scanner ET105 in vehicle systems.
Methods
This retrospective study, conducted within a single healthcare trust, analyzed data from 455 patients who underwent DaT scans for Parkinsonism investigation between January 1, 2014, and December 31, 2021. Data points included patient demographics, clinical assessment dates, scan reports, diagnoses before and after the scan, and clinical management strategies.
Results
The average age of patients at the time of scanning was 70.5 years, with 57% being male. Abnormal DaT scan results were observed in 40% of patients (n=184), while 53% (n=239) had normal scans, and 7% (n=32) showed equivocal findings. Initial clinical diagnoses aligned with DaT scan results in 71% of neurodegenerative Parkinsonism cases and 64% of non-neurodegenerative Parkinsonism cases. Across all DaT scans, a change in diagnosis occurred in 37% of patients (n=168), and clinical management was modified for 42% (n=190). Management changes included initiating dopaminergic medication in 63% of cases, discontinuing such medication in 5%, and implementing other management adjustments in 31%.
Conclusion
DaT scan imaging is a valuable tool for refining diagnosis and guiding clinical management in patients with uncertain Parkinsonism. Pre-scan diagnoses generally showed good consistency with scan outcomes. Just as an OBD scanner ET105 helps pinpoint issues in vehicle systems, DaT scans offer a more precise diagnostic pathway for neurological conditions like Parkinsonism, leading to more targeted and effective patient care.
Keywords: Parkinsonism, Dopamine transporter scan, Transporter single photon emission computed tomography, Diagnosis, Clinical management, obd scanner et105
Introduction
Parkinson’s disease (PD) is characterized by the degeneration of dopamine-producing neurons, leading to a neurodegenerative movement disorder. Clinical diagnosis is typically the first step, often guided by the UK Parkinson’s Disease Society Brain Bank Criteria, which emphasizes bradykinesia along with tremor, rigidity, or postural instability, after excluding other potential causes [1].
However, distinguishing neurodegenerative Parkinsonian disorders from non-degenerative forms of Parkinsonism, such as vascular or drug-induced Parkinson’s, or tremors like essential tremor, remains a significant clinical challenge [2]. The spectrum of conditions mimicking PD can be broad. Studies indicate that even movement disorder specialists achieve approximately 79.6% accuracy in clinically diagnosing PD, with a slight improvement to 82.7% when employing established diagnostic criteria [3]. These figures suggest that relying solely on clinical assessment may result in a considerable rate of misdiagnosis [3].
Dopamine transporter (DaT) 123I-FP-CIT single photon emission computed tomography (SPECT) is an advanced imaging technique used to differentiate neurodegenerative Parkinsonian syndromes, which involve dopamine deficiency, from other causes of Parkinsonism. DaT-SPECT demonstrates high diagnostic efficacy, with sensitivity up to 90% and specificity up to 92% in distinguishing idiopathic PD from non-neurodegenerative Parkinsonism [4]. Similar to how an OBD scanner ET105 provides specific data about a vehicle’s engine, DaT-SPECT offers detailed insights into brain dopamine transporter function.
Recent research, including a systematic review and meta-analysis, highlights that DaT scans contribute to diagnostic changes in nearly one-third of patients and management modifications in about half of those scanned [5]. Despite these findings, the review points out a gap in research, specifically limited subgroup analysis when evaluating the impact of DaT scans on clinical management [5].
This study aims to evaluate the influence of DaT scans on both diagnosis and clinical management of suspected Parkinsonian Syndrome within a movement disorder service from 2014 to 2021. The investigation includes subgroup analysis based on the clinical indication for the scan, as well as an examination of the time interval between scan acquisition and treatment initiation. This temporal analysis is crucial to better understand how DaT scan results translate into practical changes in patient management.
Methods
This retrospective study was conducted at a well-established Parkinson’s outpatient service within Northumbria Healthcare NHS Foundation Trust. The study population comprised all patients who underwent a DaT scan under the Parkinson’s service between January 1, 2014, and December 31, 2021. A comprehensive list of all DaT scans performed on patients under the trust was compiled, and patients who did not receive their DaT scan within the Parkinson’s service were excluded. This exclusion was necessary because DaT scans performed by other specialties often served different clinical purposes unrelated to movement disorders. For instance, DaT scans performed in psychiatric settings to differentiate psychiatric disorders without movement disorder features were excluded. Further exclusion criteria included insufficient clinical notes or loss to follow-up, which prevented the determination of primary outcomes. An independent clinician (KT), not directly involved in the patient care within the Parkinson’s service, reviewed electronic clinical notes to gather any necessary additional information.
Data collection encompassed patient demographics, clinical assessment dates, scan dates, scan report dates, clinical indications (pre-scan diagnosis), scan report results, post-scan diagnoses, and clinical management strategies. Clinical indications were categorized into PD, Parkinson’s Plus Syndromes, Lewy body dementia (LBD), Drug-Induced Parkinson’s (DIP), Vascular Parkinson’s (VP), Essential Tremor (ET), and other conditions. Scan outcomes were classified into three categories: abnormal (positive scan), normal (negative scan), and equivocal.
Parkinson’s Plus Syndromes included progressive supranuclear palsy (PSP), multiple system atrophy, and corticobasal degeneration. The ‘other conditions’ category comprised ventroperitoneal shunt, normal pressure hydrocephalus, cerebral myelomalacia/encephalomalacia, and anxiety-induced tremor. Changes in clinical management were defined as initiation of treatment, alteration in treatment dose or type, or cessation of treatment following the scan result. Patients continuing on the same treatment or not initiating treatment were classified as having no change in clinical management.
Referrals for DaT scans were made by movement disorder specialists when diagnostic uncertainty existed or diagnostic confirmation was required. The DaT scans were performed by an independent radiology department, separate from patient management decisions. Institutional review board approval was secured before commencing data collection.
Results
Between 2014 and 2021, the Parkinson’s team requested a total of 455 DaT scans. A slight majority of patients were male (57%), and the mean age at scanning was 70.5 years (range 36–90 years). Annual analysis showed a trend of increasing average age at DaT scan receipt from 2014 to 2021. In all years, males constituted the majority. The median time from clinical assessment to DaT scan report availability was 35 days. Table 1 details basic patient demographics from 2014 to 2021.
Table 1.
Basic patient demographic from 2014 to 2021
| Demographics | 2014 | 2015 | 2016 | 2017 | 2018 | 2019 | 2020 | 2021 | Total |
|---|---|---|---|---|---|---|---|---|---|
| Mean age (years) | 68.8 | 66.8 | 65.3 | 65.0 | 72.9 | 72.4 | 71.6 | 74.2 | 70.5 |
| Male (n) | 29 | 30 | 27 | 13 | 26 | 55 | 33 | 46 | 259 |
| Female (n) | 22 | 25 | 22 | 8 | 18 | 32 | 25 | 43 | 195 |
| Male (%) | 56.9 | 54.5 | 55.1 | 61.9 | 59.1 | 63.2 | 55.9 | 51.7 | 56.9 |
| Female (%) | 43.1 | 45.5 | 44.9 | 38.1 | 40.9 | 36.8 | 44.1 | 48.3 | 42.9 |
| Number of scans (n) | 51 | 55 | 49 | 22 | 44 | 87 | 58 | 89 | 455 |
The distribution of scan results was as follows: 184 patients (40%) had abnormal scans, 239 (53%) had normal scans, and 32 (7%) had equivocal scans.
Pre-scan diagnosis outcomes
Suspected idiopathic PD was the most frequent pre-scan diagnosis, accounting for 190 scans (42%), followed by suspected ET (129 scans, 29%) and DIP (45 scans, 10%). The total number of patients included in this analysis was 451. Pre-scan diagnosis was undetermined in four scans (1%) due to insufficient clinical record information, and these were excluded from this part of the analysis. Among patients with a pre-scan diagnosis of PD, 100 (54%) had abnormal DaT scans, representing the largest proportion within this group. For patients with a pre-scan diagnosis of ET, 105 (44%) had normal scans. Table 2 provides a detailed breakdown of DaT scan numbers and percentages by pre-scan diagnosis and subsequent scan outcomes.
Table 2.
The number and percentage of scans stratified by the pre-scan diagnosis from 2014 to 2021
| Pre-scan diagnosis | Number of abnormal scans | Abnormal scans (%) | Number of normal scans | Normal scans (%) | Number of equivocal scans | Equivocal scans (%) | Total number of scans (pre-scan diagnosis) |
|---|---|---|---|---|---|---|---|
| Possible PD | 100 | 55.2 | 74 | 31.1 | 16 | 50.0 | 190 |
| ET | 16 | 8.8 | 105 | 44.1 | 8 | 25.0 | 129 |
| LBD | 18 | 9.9 | 8 | 3.4 | 2 | 6.3 | 28 |
| DIP | 11 | 6.1 | 31 | 13.0 | 3 | 9.4 | 45 |
| Parkinson’s plus | 13 | 7.2 | 2 | 0.8 | 1 | 3.1 | 16 |
| VP | 13 | 7.2 | 11 | 4.6 | 2 | 6.3 | 26 |
| Other diagnosis | 10 | 5.5 | 7 | 2.9 | 0 | 0 | 17 |
| Total number of scans (scan outcome) | 181 | 238 | 32 | ||||
| Grand total of scans | 451 |
PD Parkinson’s disease, ET essential tremor, LBD Lewy-body dementia, DIP Drug-induced Parkinsonism, VP vascular parkinsonism
Bold values indicate the total number of scans (raw number)—It is calculated by the number of abnormal scnas+number of normal scans and number of equivocal scans in that row
Pre-scan diagnoses suggestive of abnormal DaT scan results included PD, LBD, and Parkinson’s plus syndromes. Among the 181 patients with abnormal scans, 131 (73%) had a pre-scan diagnosis consistent with the scan result. Of the 238 patients with normal scans, 154 (65%) had pre-scan diagnoses aligning with the DaT scan outcome (including ET, DIP, VP, and other diagnoses).
Post-scan diagnosis and clinical management
Considering all DaT scans, diagnosis was altered for 168 patients (37%), and clinical management changed for 190 patients (42%). Conversely, diagnosis remained unchanged in 283 patients (63%), and clinical management was unaltered in 260 patients (58%). Information regarding diagnosis and clinical management was insufficient for four and five patients, respectively.
Among abnormal scans, 66 (37%) resulted in a diagnostic change, and 118 (65%) led to a clinical management change. For normal scans, 91 (38%) prompted a diagnostic change, while 51 (22%) resulted in management changes. Equivocal scans led to diagnostic changes in 15 patients (36%) and management changes in 13 (62%). Table 3 details the number and percentage of patients experiencing changes in diagnosis and management.
Table 3.
The number and percentage of people with a change in diagnosis and management stratified by the pre-scan diagnosis from 2014 to 2021
| Pre-scan diagnosis | Number of patients with a change in diagnosis | Patients who had a change in diagnosis (%) | Number of patients with a change in management | Patients who had a change in management (%) |
|---|---|---|---|---|
| Possible PD | 98 | 55.7 | 87 | 45.3 |
| ET | 30 | 17.0 | 52 | 27.1 |
| LBD | 10 | 5.7 | 12 | 6.3 |
| DIP | 17 | 9.7 | 14 | 7.3 |
| Parkinson’s plus | 5 | 2.8 | 9 | 4.7 |
| VP | 5 | 2.8 | 11 | 5.7 |
| Other diagnosis | 11 | 6.3 | 7 | 3.6 |
| Total number of scans as per scan result | 176 | 192 |
PD Parkinson’s disease, ET essential tremor, LBD Lewy-body dementia, DIP Drug-induced Parkinsonism, VP vascular parkinsonism
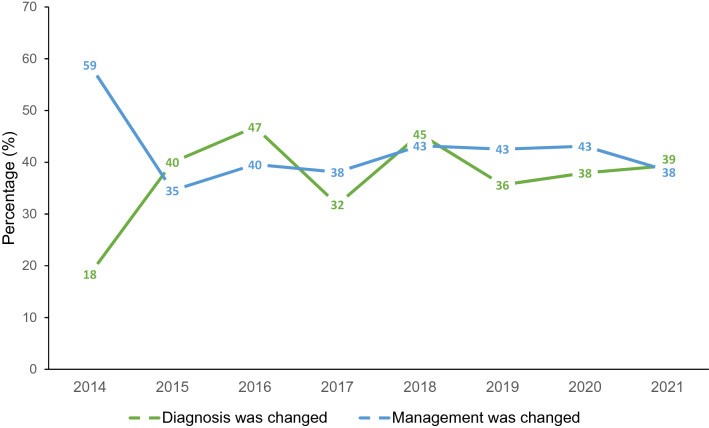
Among patients with management changes, 119 (63%) initiated dopaminergic medication. Dopaminergic medication was discontinued in 10 patients (5%), and 58 patients (31%) experienced other management changes, including starting medication for ET or LBD, stopping medications causing DIP, or referral to other specialists. Figure 1 illustrates the trends in diagnostic and clinical management changes over the study period.
Fig. 1.
Alt text: Graph showing percentage trends of changes in diagnosis and clinical management following DaT scans from 2014 to 2021, highlighting the impact of diagnostic tools like DaT scans, in contrast to vehicle diagnostic tools such as OBD scanner ET105.
Percentage of change in diagnosis and clinical management from DaT scans from 2014 to 2021
Analysis of the time from DaT scan report to treatment initiation, available for 2018–2021 (278 scans), showed a mean duration of 167 days and a median of 91 days.
Historical data
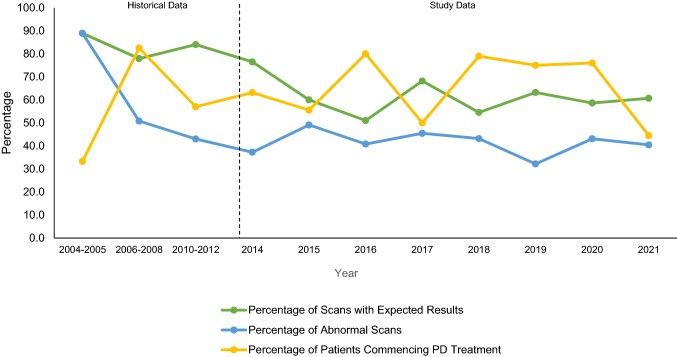
Historical data since 2004 indicate an increase in DaT scan usage, from an average of 9 scans per year in 2004–2005, to 21 in 2006–2008, and 78 in 2010–2012. Data for 2009 and 2013 were unavailable.
In 2004–2005, 16 patients (89%) had scan results confirming initial diagnoses, 16 scan results (89%) were abnormal, and 6 patients (33%) started treatment. In 2006–2008, 49 patients (78%) had scan results consistent with expected diagnoses, 32 scans (51%) were abnormal, and 52 patients (83%) initiated treatment. In 2010–2012, 197 patients (84%) had scan results confirming initial diagnoses, 101 scans (43%) were abnormal, and 134 patients (57%) started treatment.
Table 4 summarizes scan numbers per year, percentage of scans confirming expected diagnoses, abnormal scan percentages, and treatment initiation percentages for both historical and study data. Figure 2 graphically represents trends in these percentages.
Table 4.
The number of scans per year, the percentage of scan results that matched the expected diagnosis, the percentage of positive scans, and the percentage of those starting treatment, for both historical and study data
| Time period | Historical data | Study data |
|---|---|---|
| 2004–2005 | 2006–2008 | |
| Number of scans | 18 | 63 |
| Scans per year (average number of scans for historical data) | 9 | 21 |
| Number of scans with expected results | 16 | 49 |
| Number of abnormal scans | 16 | 32 |
| Number of patients commencing PD treatment | 6 | 52 |
| Scans with expected results (%) | 88.9 | 77.9 |
| Abnormal scans (%) | 88.9 | 50.8 |
| Patients commencing PD treatment (%) | 33.3 | 82.5 |
Fig. 2.
Alt text: Line graph illustrating trends over time for percentages of DaT scan results matching expected diagnoses, abnormal scan rates, and Parkinson’s disease treatment initiation rates, emphasizing the evolution of diagnostic imaging similar to advancements in tools like OBD scanner ET105.
Trends in percentages for scan results that matched the expected diagnosis, percentages of abnormal scans, and percentages of patients starting PD treatment, for both historical and study data
Discussion
This study aimed to evaluate the application of DaT scans in diagnosing and managing patients exhibiting Parkinsonism where the underlying cause was clinically ambiguous.
Over the years studied, the average patient age at DaT scanning has increased, and males consistently represented the majority (57%). The higher prevalence of PD and ET in males likely contributes to this observation [6, 7].
Pre-scan diagnosis subgroups
Clinical pre-scan diagnoses generally showed good agreement with DaT scan results. For neurodegenerative Parkinsonism, pre-scan diagnoses were consistent with scan results in 72% of cases. For non-neurodegenerative Parkinsonism, this consistency was 65%.
Reported consistency rates between pre-scan diagnoses and DaT scan results vary. A prospective study noted poor correlation, with 36% discordance for pre-synaptic Parkinson’s syndromes and 54% for non-pre-synaptic Parkinson’s syndromes [8]. This aligns partially with our findings, showing higher congruence for neurodegenerative versus non-neurodegenerative Parkinsonism, although our study showed higher overall agreement. Another study reported a 65% agreement for non-neurodegenerative diagnoses, closely mirroring our results [9].
Post-scan diagnosis and management
This study demonstrated clinically significant changes in diagnosis and management resulting from DaT scan use. Diagnosis changed in 37% of patients, and management in 42%, consistent with existing literature [5, 10–12]. A 30% threshold has been previously used to define clinically significant outcome changes, as seen in positron emission tomography studies for dementia and cognitive impairment and adopted by a systematic review on DaT scan impacts [5, 13]. Our findings further support the clinical significance of DaT scans in diagnosing and managing these patients.
Among abnormal scans, 37% led to diagnostic changes and 65% to management changes, exceeding the clinical significance threshold. However, for normal scans, while 38% caused diagnostic changes, only 22% altered management. This is expected, as a negative scan typically rules out neurodegenerative Parkinsonism, reducing the necessity for dopaminergic treatment. Treatment decisions are ultimately based on the specific condition, symptom severity, and disease progression. Non-neurodegenerative movement disorders like VP and DIP are often not treated with dopaminergic medications due to limited evidence of benefit and potential harm from side effects [14–16]. For ET, patients may opt out of treatment if symptoms are not significantly disruptive [17].
Equivocal scans resulted in diagnostic changes in 33% and management changes in 67% of cases. Clinicians often provide a most-likely differential diagnosis when requesting scans. A change from this diagnosis post-scan was considered a diagnostic change. The higher proportion of management changes compared to diagnostic changes may reflect the use of DaT scans to confirm suspected diagnoses rather than identify alternate pathologies [5].
Patients with equivocal scans typically did not undergo repeat scans but were clinically followed up and assessed for treatment response, which often aided in diagnosis based on clinical progression. Their outcomes more closely resembled those with abnormal scans. Long-term outcome studies for patients with equivocal scans are warranted.
Consistent with existing literature, management changes were more frequent than diagnostic changes across all subgroups, potentially reflecting the confirmatory role of DaT scans in clinical practice [5].
Duration to starting treatment
Between 2018 and 2021, the average time to treatment initiation was 167 days, with a median of 91 days. The discrepancy suggests outliers with delayed treatment initiation even after positive DaT scans. In Parkinson’s disease, treatment is primarily for symptomatic control and quality of life improvement, as current treatments do not slow disease progression [18]. A randomized trial showed that delaying treatment by 40 weeks did not negatively impact Parkinsonian symptoms [19]. The study also found no benefit or disadvantage to early versus delayed levodopa initiation, addressing previous concerns about potential neurotoxicity or neuroprotection [18–20]. The observed treatment delays in our study reflect current clinical evidence, with treatment initiation guided by patient clinical and symptomatic needs rather than solely by scan results. These delays also highlight the influence of other factors in management planning.
However, this is pertinent only to patients initiating treatment post-scan. Negative DaT scans remain valuable in ruling out neurodegenerative disease, facilitating access to alternative treatments or enabling cessation of unnecessary dopaminergic medication, especially given the well-documented side effects of PD medications [21].
Furthermore, negative DaT scans facilitate the identification of patients suitable for discharge from Parkinson’s services, alleviating clinical pressures and improving service accessibility for new patients.
Historical data
DaT scans were introduced in our service in 2004, with usage increasing until 2010, after which it stabilized, likely due to routine integration and increased clinician experience with their utility.
Scans consistently confirmed expected diagnoses, even early on, underscoring their confirmatory role. Fluctuations in dopaminergic medication initiation rates over time are observed, as treatment decisions are not solely scan-dependent. Despite variability, over 30% of patients commenced dopaminergic medication across all assessed years, suggesting a clinically significant impact of DaT scanning since 2004, based on the previously mentioned threshold.
Excluding 2004–2005, abnormal scan percentages remained relatively stable between 30% and 50% (Fig. 2). The higher abnormal scan rate in 2004–2005 (89%) is likely due to the low scan volume in early implementation and clinicians’ potentially higher threshold for suspicion of neurodegenerative Parkinsonism before scanning, especially before the UK National Institute of Health and Care Excellence guidelines in 2006 [22]. These guidelines likely clarified DaT scan usage, explaining the subsequent increase in scans and improved consistency in scan results aligning with initial diagnoses from 2006 onwards.
Strengths and limitations
This study benefits from a large single-center cohort, enhancing its power to assess DaT scan utility in clinically uncertain Parkinsonism. It also addresses under-reported outcomes like the time to treatment initiation, providing practical insights into clinical management.
The service, while geriatrician-led, is not age-restricted and serves a large proportion (>85%) of PD patients in the Northumbria catchment area [23, 24], strengthening the study’s representativeness.
Limitations include the retrospective design, leading to missing data for some patients and potential attrition bias. Lack of initial documentation meant pre-scan diagnoses were indeterminable for a few patients, and loss to follow-up caused missing post-scan outcome data.
Single-center design limits generalizability. The study did not assess clinician-specific scan request variations over time due to experience, which could introduce variability in clinical uncertainty thresholds.
Clinicopathological correlation with post-mortem data was not performed due to most patients being alive, but this is a potential future research area.
Finally, while DaT scans significantly contribute to diagnostic and management decisions, quantifying their precise influence on management changes is challenging, as management plans involve multiple factors beyond scan results, such as symptom severity, quality of life, patient preferences, and medication contraindications.
Conclusion
This study concludes that DaT imaging is a valuable tool for supporting accurate diagnosis and clinical management in patients with clinically uncertain Parkinsonism. Clinician pre-scan diagnoses showed reasonable consistency with DaT scan results. However, treatment plans were not always immediately implemented post-scan, likely influenced by factors like disease severity and impact. Further research should evaluate DaT scan impacts on patient outcomes, including quality of life and symptom control. Similar to how advanced diagnostic tools like OBD scanner ET105 refine vehicle maintenance, DaT scans enhance the precision of neurological care.
Author contributions
Research project: A. conception, B. organization, and C. execution; statistical analysis: A. design, B. execution, C. Review and critique; manuscript preparation: A. writing of the first draft, and B. review and critique; KT: 1A, 1B, 1C, 2A, 2B, 2C, 3A, 3B. RW: 1A, 1B, 2A, 2C, 3B.
Funding
No specific funding was received for this work.
Data availability
The participants of the study did not give written consent for their data to be shared publicly. Additionally, due to the confidential nature of the research data, the supporting data for this research is not available.
Declarations
Conflicts of interest
KT has no competing interests for this work. Within the past year, RW has provided a meeting presentation for the BIAL advisory board, in topics unrelated to this research.
Ethical standard statement
Institutional approval for this study was granted by Northumbria Healthcare NHS Foundation Trust. RW acted as the Caldicott Guardian for this study to ensure correct handling of confidential data. Informed patient consent was not necessary for this work. We confirm that we have read the Journal’s position on issues involved in ethical publication and affirm that this work is consistent with those guidelines.
References
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The participants of the study did not give written consent for their data to be shared publicly. Additionally, due to the confidential nature of the research data, the supporting data for this research is not available.
