Introduction
Depression stands as a pervasive mental health challenge in the United States, impacting millions of adults. Recognized as a leading cause of disability, it carries significant personal and economic burdens. The urgency to address this issue is underscored by the U.S. Preventive Services Task Force (USPSTF) recommendation for universal depression screening in primary care settings. Leveraging effective Depression Screening Tools Primary Care Screener For Affective Disorder becomes paramount in early detection and intervention. This article explores the critical role of primary care in identifying and managing depression, focusing on the implementation of measurement-based care (MBC) programs to improve patient outcomes. We delve into the effectiveness of such programs, using the VitalSign6 project as a case study, to highlight the transformative potential of systematic depression screening in primary care.
The Undeniable Impact of Depression
Depression is not just a fleeting feeling; it is a significant public health concern. Affecting an estimated 17.3 million US adults annually, depression manifests as more than just sadness. It’s a complex disorder that disrupts daily life, diminishes productivity, strains relationships, and significantly increases the risk of comorbid physical health conditions. The economic toll is staggering, estimated at $210 billion each year in medical costs and lost productivity. Untreated depression perpetuates a cycle of suffering, emphasizing the critical need for effective identification and intervention strategies within primary care. Recognizing depression as an affective disorder that can be effectively screened for is the first step in mitigating its widespread impact.
Primary Care: The Frontline for Depression Screening
Primary care settings are uniquely positioned to address the challenge of undiagnosed and undertreated depression. Recommendations from the USPSTF and endorsements from organizations like the American Academy of Family Physicians emphasize the importance of routine depression screening for adults in these settings. Furthermore, value-based payment models from Centers for Medicare & Medicaid Services (CMS) are increasingly incentivizing depression screening and follow-up care within accountable care organizations. The landmark STAR*D trial further solidifies this approach, demonstrating that depression treatment initiated in primary care can achieve outcomes comparable to specialty mental health care. Despite this compelling evidence and widespread recommendations, depression screening rates remain surprisingly low, highlighting a significant gap between guidelines and actual clinical practice. Improving the utilization of primary care depression screening tools is crucial to bridging this gap and ensuring timely access to care.
Bridging the Gap: The Role of Effective Screening Tools
The under-recognition and undertreatment of depression in primary care necessitates a focus on enhanced screening practices. Depression screening tools, particularly the Patient Health Questionnaire (PHQ)-2 and PHQ-9, have emerged as reliable and validated instruments for this purpose. The PHQ-2 serves as an efficient initial screen, prompting further assessment with the more comprehensive PHQ-9 when indicated. These tools, based on DSM-5 criteria for major depressive disorder, offer a standardized and quantifiable approach to identifying potential cases of depression. Meta-analyses have consistently confirmed the effectiveness of both PHQ-2 and PHQ-9 in detecting depression within primary care populations. The integration of these affective disorder screening tools into routine primary care workflows is a key step towards improving identification rates.
Measurement-Based Care: A Systemic Approach to Depression Management
Beyond simply screening, effective depression care requires a systematic approach to treatment and follow-up. Measurement-based care (MBC) provides this framework, integrating validated depression screening tools, standardized symptom measurements, and evidence-based decision support. MBC empowers primary care physicians with the resources needed for accurate diagnosis, tailored treatment planning, and ongoing monitoring of patient progress. This comprehensive approach includes established protocols for referrals to specialty care when necessary. The VitalSign6 program, developed by The University of Texas Southwestern Medical Center for Depression Research and Clinical Care (CDRCC), exemplifies MBC in action. By leveraging technology to seamlessly integrate screening and MBC into electronic health records (EHRs), programs like VitalSign6 are paving the way for more efficient and effective depression care in primary care.
VitalSign6: Implementing Measurement-Based Care in a Primary Care Setting
To demonstrate the practical application of MBC, a quality improvement project was undertaken to implement VitalSign6 within the Department of Family and Community Medicine at the University of Texas Southwestern Medical Center (UTSW). The project aimed to improve depression identification and management among adult patients by integrating VitalSign6 into the clinic’s existing workflow.
Specific Aims:
- Achieve a 75% screening rate for depression using PHQ-2 among unique patients.
- Ensure 85% of PHQ-2 positive patients are further screened with PHQ-9.
- Administer MBC to 75% of patients diagnosed with depression, including scheduled follow-up.
- Utilize VitalSign6 MBC to monitor treatment responses and remission.
- Evaluate physician and staff satisfaction with VitalSign6 and EHR integration.
These aims were derived from the VitalSign6 Primary Care First Model, reflecting established benchmarks for effective depression screening and MBC implementation.
Methodology: A Pre-Post Intervention Design
The project employed a pre-post intervention design to assess the impact of VitalSign6 implementation on screening rates, clinical outcomes, and satisfaction. The setting was a busy primary care clinic within UTSW, characterized by a residency program and a diverse patient population. The project spanned several months, encompassing initial screening and subsequent follow-up for patients diagnosed with depression. Ethical approval was obtained from the UTSW Institutional Review Board.
Innovation: VitalSign6 and EHR Integration
VitalSign6 is a web-based MBC program designed to provide primary care providers with tools for standardized assessment of depression symptoms, medication side effects, and treatment adherence. It also offers algorithm-based decision support for medication selection and dosing. A key innovation of this project was the development of an application programming interface (API) that enabled real-time integration of VitalSign6 with the clinic’s Epic EHR system. This integration streamlined workflow, allowing physicians to launch VitalSign6 directly within Epic, review patient data, access decision support tools, and seamlessly document treatment plans within the patient chart. This interoperability addressed a critical barrier to technology adoption in healthcare settings.
Figure 1. VitalSign6 Integration with Epic
Figure 1: This image illustrates the seamless integration of VitalSign6 with the Epic Electronic Health Record (EHR) system, highlighting how patient data and clinical decision support tools are readily accessible to providers within their existing workflow.
Training and Engagement: Setting the Stage for Success
Successful implementation required comprehensive training and stakeholder engagement. Two-hour in-person training sessions were conducted for physicians, residents, and clinic staff, covering depression education, screening protocols, MBC principles, and the use of VitalSign6. On-site support from VitalSign6 experts was provided for two weeks post-training to ensure a smooth transition and address any initial challenges.
Procedures: From Initial Screening to Follow-Up
Initial Screening: Patients completed the PHQ-2 on tablets during check-in. Positive screens or a history of depression triggered a PHQ-9 assessment via VitalSign6 on iPads. Self-reported scores were automatically integrated into the EHR, providing physicians with real-time access to screening results.
Follow-up Visits: At follow-up appointments, patients repeated the PHQ-9 and other relevant measures through VitalSign6. Physicians utilized decision support tools within VitalSign6 to guide treatment adjustments, schedule further follow-up, or facilitate specialist referrals based on patient progress.
Satisfaction Assessment: Pre- and post-implementation surveys, using Likert-type scales, were administered to physicians and staff to assess their satisfaction with depression care and their perceptions of VitalSign6. Open-ended questions in the post-survey explored the perceived challenges and valuable aspects of using VitalSign6.
Outcome Measures and Data Analysis
Program fidelity was assessed by tracking screening rates and MBC administration. Clinical outcomes were measured by changes in patient PHQ-9 scores from baseline to follow-up. Physician and staff satisfaction were evaluated using the survey data. Statistical analyses, including paired t-tests and Mann-Whitney U tests, were conducted to compare pre- and post-intervention data.
Results: Improved Screening and Patient Outcomes
Enhanced Screening Rates and Sample Demographics
During the project period, an impressive 95.4% of the 1200 unique adult patients visiting the clinic were screened for depression using PHQ-2. Of those screened, 18.2% screened positive on the PHQ-2, and a significant majority (89.4%) of these positive screens were followed up with PHQ-9 assessments. The patient sample was diverse, reflecting the demographics of a typical primary care setting.
Depression Follow-Up and Treatment Pathways
Of the patients screened with PHQ-9, 62.8% screened positive, leading to a diagnosis of depressive disorder in 89.4% of these cases. The majority of diagnosed patients (87.4%) initiated MBC with personalized treatment plans, while a smaller percentage were referred to specialty care or declined treatment. Pharmacological treatment was the most common intervention, followed by non-pharmacological approaches and symptomatic monitoring. Patients were followed for 14 weeks to assess treatment response.
Figure 2. CONSORT Flow Diagram
Figure 2: This CONSORT flow diagram visually summarizes the patient progress through the depression screening and treatment process, from initial screening to follow-up, illustrating patient flow and attrition rates.
Significant Reduction in Depression Scores
A paired t-test analysis of 65 patients with complete data revealed a statistically significant decrease in self-reported PHQ-9 scores from baseline to follow-up. The mean PHQ-9 score dropped from 14.89 to 9.58, indicating a positive clinical impact of the MBC intervention. Furthermore, 23.1% of these patients achieved remission, defined as a PHQ-9 score below 5.
Figure 3. PHQ-9 Scores at Baseline and Follow-Up
Figure 3: This graph visually compares the distribution of PHQ-9 scores at baseline and follow-up, demonstrating the shift towards lower scores and improved patient outcomes after the intervention.
Physician and Staff Perceptions: Mixed Feedback
Physician surveys indicated a statistically significant decrease in their perceived importance of depression screening and MBC post-implementation, a surprising finding potentially linked to workflow disruptions caused by technology integration challenges. Staff surveys, however, showed a significant improvement in their comfort level discussing mental health with patients. Open-ended survey responses highlighted both challenges, primarily workflow slowdown and technical issues, and valuable aspects, such as EHR integration and improved screening awareness.
Table 1. Provider Survey Results
| Provider survey items | Pre, median (min, max) | Post, median (min, max) | P |
|---|---|---|---|
| How frequently are you currently treating depression? | 4.5 (3, 5) | 4 (3, 5) | .466 |
| My current understanding of depression is: | 4 (3, 5) | 4.5 (3, 5) | .912 |
| Depression is a chronic medical illness. | 5 (3, 5) | 4.5 (3, 5) | .217 |
| Depression in primary care patients is common. | 5 (4, 5) | 5 (4, 5) | .287 |
| Depression should mostly be treated by psychiatrists. | 1 (1, 5) | 2 (1, 3) | .494 |
| Primary care is the best setting to screen for depression. | 5 (3, 5) | 4 (3, 5) | .051 |
| When treating depression, it is important to use measures to assess symptoms. | 5 (4, 5) | 4 (3, 5) | .002 |
| I believe that it is important to screen patients for depression in my clinic. | 5 (4, 5) | 4 (4, 5) | .002 |
| I can accurately diagnose patients who screen positive for depression. | 4 (3, 5) | 4 (4, 5) | .328 |
| I am very familiar with how to use antidepressant medications. | 4 (2, 5) | 4 (1, 5) | .471 |
| I feel confident in knowing when to change antidepressant medications. | 4 (2, 5) | 4 (1, 4) | .270 |
| I know what medications can be used to augment an antidepressant medication. | 4 (2, 5) | 4 (1, 4) | .562 |
| I feel comfortable talking with my patients about their mental health. | 5 (3, 5) | 4.5 (4, 5) | .474 |
| How easy is the VitalSign6 software program to use with your daily workflow? | na | 2.5 (1,4) | nc |
| How easy is the VitalSign6 software program to use in the presence of patients? | na | 2.5 (1, 4) | nc |
| Overall, how easy is the VitalSign6 software program to use? | na | 3 (2, 4) | nc |
| How useful is the VitalSign6 software program in following a patient’s status over time? | na | 3.5 (1, 4) | nc |
| How useful do you find the treatment recommendations (clinical decision support)? | na | 1.5 (1, 4) | nc |
| Overall, how useful is the VitalSign6 software program? | na | 3 (1, 4) | nc |
| How often does the VS6 software program draw your attention to issues or problems? | na | 3.5 (2, 5) | nc |
| To what extent has VitalSign6 program improved the quality of patient care? | na | 3 (1, 4) | nc |
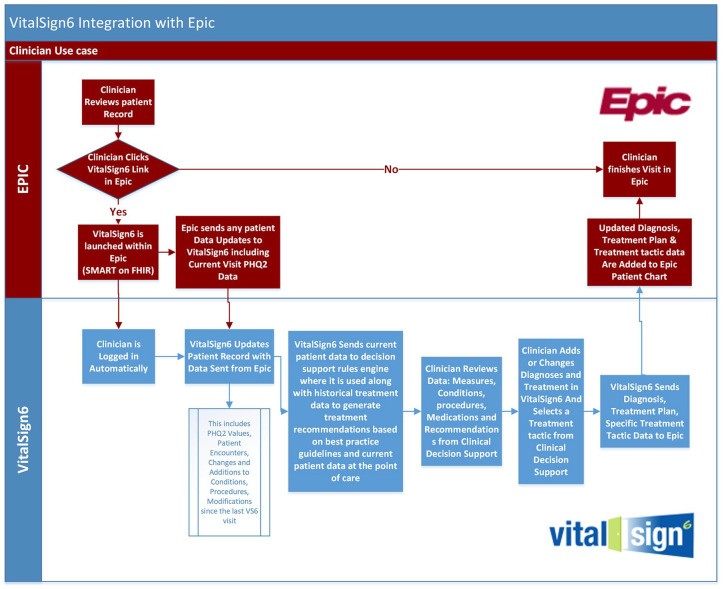
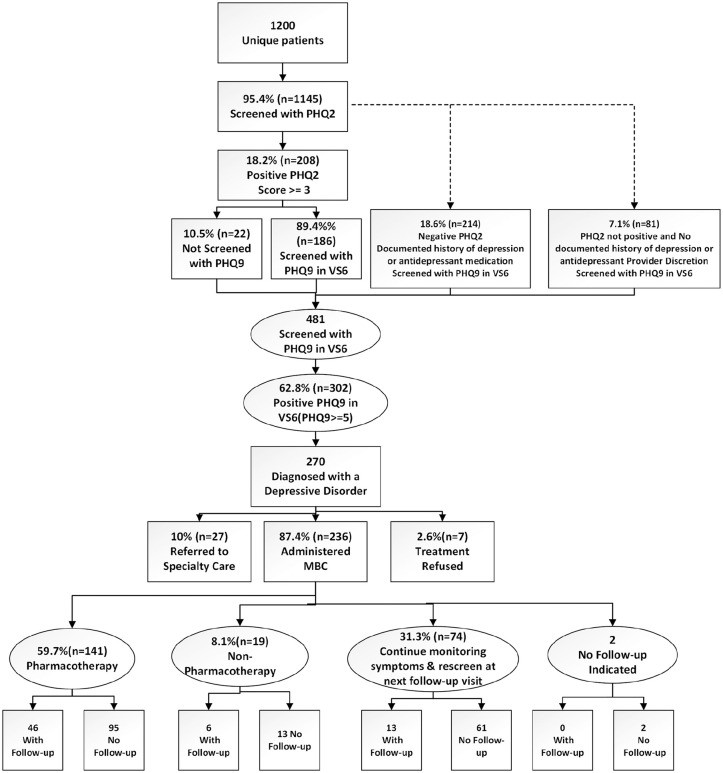
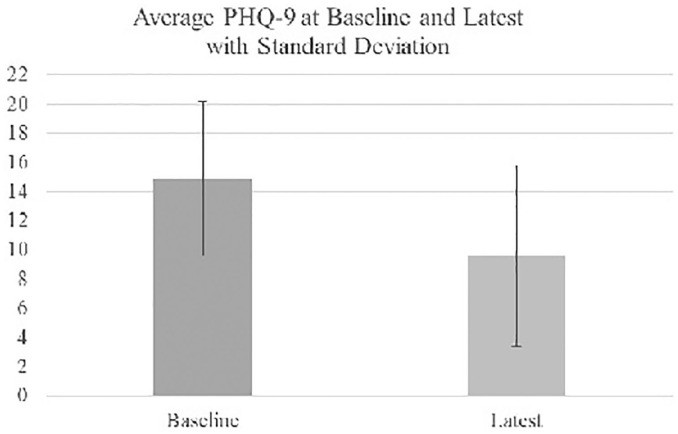
Table 2. Staff Survey Results
| Staff survey items | Pre, median (min, max) | Post, median (min, max) | P |
|---|---|---|---|
| My current understanding of depression is: | 3 (3, 5) | 4 (3, 5) | .362 |
| Depression is a chronic medical illness. | 4 (3, 5) | 4.5 (2, 5) | .935 |
| Depression in primary care patients is common. | 4 (3, 5) | 4 (4, 5) | .622 |
| Depression should mostly be treated by psychiatrists. | 3 (2, 5) | 2 (1, 5) | .057 |
| Primary care is the best setting to screen for depression. | 4 (2, 5) | 4.5 (3, 5) | .080 |
| I believe that it is important to screen patients for depression in my clinic. | 4 (3, 5) | 4.5 (3, 5) | .083 |
| I feel comfortable talking with my patients about their mental health. | 3 (1, 4) | 4 (1, 5) | .044 |
| How easy is the VitalSign6 software program to use with your daily workflow? | — | 2.5 (1, 5) | — |
| Overall, how easy is the VitalSign6 software program to use? | — | 3 (2, 5) | — |
| Overall, patients are receptive to depression screening using the VitalSign6 software. | — | 2 (1, 4) | — |
| To what extent does your role contribute to patients receiving quality care? | — | 3.5 (2, 5) | — |
Discussion: VitalSign6 as an Effective Adjunct
The project demonstrated that implementing VitalSign6 significantly improved depression screening rates and patient remission rates within a primary care setting. The observed remission rate of 23.1%, a notable improvement from the baseline, underscores the positive impact of combining systematic screening with measurement-based care and EHR-integrated clinical decision support tools. The findings support the concept of depression care as a triageable condition within primary care, rather than solely a mental health access issue. VitalSign6 equipped primary care providers to effectively manage a large proportion of diagnosed patients, reducing the need for specialist referrals. While physician satisfaction surveys revealed concerns about workflow disruptions, staff comfort in addressing mental health improved, highlighting the importance of comprehensive training and ongoing support during technology implementation.
Addressing Workflow and Technology Integration
The challenges related to workflow and technology integration emphasize the need for careful planning and iterative refinement during EHR system implementations. The initial requirement for using Epic Welcome tablets, coupled with technical interoperability issues, likely contributed to physician frustrations and the unexpected decrease in perceived importance of screening. Future efforts should prioritize seamless integration, bidirectional data flow, and user-friendly interfaces to minimize workflow disruptions and maximize the benefits of MBC programs. Upcoming EHR upgrades and further optimization of VitalSign6 integration hold promise for addressing these challenges.
Limitations and Future Directions
The study’s limitations, including its single-site design and focus on specific screening measures, warrant consideration. The high patient attrition rate for follow-up visits also highlights an area for improvement. Future research should explore strategies to enhance patient retention, such as care coordination, patient navigation, and teletherapy interventions. Expanding the scope to include other measures available within VitalSign6, such as anxiety screening and treatment adherence monitoring, would further enhance the comprehensiveness of depression care in primary care settings.
Conclusion: Advancing Depression Care in Primary Care
The VitalSign6 quality improvement project provides compelling evidence for the effectiveness of measurement-based care in improving depression identification and management within primary care. By leveraging depression screening tools primary care screener for affective disorder like PHQ-2 and PHQ-9, integrated with EHR systems and supported by robust clinical decision support, primary care practices can significantly enhance their capacity to address the mental health needs of their patients. While workflow optimization and ongoing technology refinement are essential, the results of this project contribute to a growing body of evidence supporting the widespread adoption of MBC programs like VitalSign6 to improve depression care delivery and patient outcomes in primary care. Further research and implementation efforts are needed to translate these findings into sustainable, scalable models of integrated mental health care within primary care settings.

