Depression stands as a prevalent mental health disorder across the United States, significantly impacting adults. Recognizing this widespread issue, the U.S. Preventive Services Task Force (USPSTF) advocates for routine depression screening for adults within primary care settings, emphasizing the use of evidence-based approaches. This article delves into the critical role of depression screening tools in primary care, highlighting the implementation and impact of measurement-based care programs designed to improve the identification and treatment of depression in these crucial healthcare environments.
The Imperative for Depression Screening in Primary Care
Depression is not merely a transient state of sadness; it is a clinically significant condition affecting millions. Statistics reveal that a substantial percentage of U.S. adults experience at least one major depressive episode, underscoring its widespread nature. The ramifications of untreated depression are far-reaching, encompassing emotional distress, diminished productivity, economic losses, strained interpersonal relationships, and heightened risks of co-occurring health conditions. The intricate link between mental and physical well-being further accentuates the urgency of addressing depression, especially given its frequent co-occurrence with chronic physical illnesses.
Evidence overwhelmingly supports the integration of depression screening and treatment within primary care. Early detection and intervention are paramount in mitigating the adverse effects of depression. The USPSTF guidelines recommend universal screening for adults aged 18 and above in primary care, coupled with robust support systems and evidence-based treatment protocols. These recommendations are echoed by organizations like the American Academy of Family Physicians and are increasingly incentivized by value-based payment models from Centers for Medicare & Medicaid Services (CMS), which emphasize depression screening, follow-up, and remission as key performance indicators.
The landmark STAR*D trial, a comprehensive study on depression treatment, affirmed the effectiveness of primary care settings for delivering quality depression care, comparable to specialty mental health services. Despite these compelling findings and national guidelines, a significant gap persists: over half of primary care patients with depression remain undiagnosed and undertreated. National data highlights alarmingly low rates of depression screening in primary care visits, indicating a critical need for enhanced implementation strategies.
Key Depression Screening Tools for Primary Care Settings
To bridge the gap in depression identification, the adoption of effective screening tools is essential. Among the array of available instruments, the Patient Health Questionnaire (PHQ)-2 and PHQ-9 stand out as the most widely utilized and validated depression screening tools for adults in primary care. These tools are lauded for their clinical utility and diagnostic accuracy, making them invaluable assets for primary care physicians.
The PHQ-2 serves as an efficient initial screening step. It comprises just two questions focusing on the core symptoms of depression: depressed mood and anhedonia (loss of interest or pleasure). Each item is scored on a scale from 0 (“not at all”) to 3 (“nearly every day”). A total PHQ-2 score of 3 or higher is considered a positive screen, indicating the need for further evaluation with the more comprehensive PHQ-9. Research demonstrates the PHQ-2’s strong ability to detect major depression, boasting high sensitivity and specificity.
For patients who screen positive on the PHQ-2, or when a more thorough assessment is warranted, the PHQ-9 is employed. This 9-item questionnaire directly aligns with the DSM-5 diagnostic criteria for major depressive disorder. The PHQ-9 delves deeper into the various symptom dimensions of depression, and the total score provides an indication of depression severity, ranging from mild to severe.
Image Alt Text: Primary care physician reviews depression screening results on a tablet with a patient, illustrating the integration of technology in mental health assessments within a clinic.
Meta-analyses consolidating data from thousands of primary care patients have consistently confirmed the PHQ-2 and PHQ-9 as effective, valid, and reliable instruments for depression detection in these settings. These findings underscore the importance of not only screening but also integrating screening with comprehensive systems of care to achieve optimal patient outcomes and long-term remission.
Measurement-Based Care and VitalSign6: A Systemic Approach
Beyond simply using screening tools, the concept of measurement-based care (MBC) is crucial for enhancing depression care in primary settings. MBC provides a structured framework encompassing validated screening tools, standardized symptom measurement, monitoring of treatment effects and adherence, and evidence-based decision support. This comprehensive approach empowers primary care physicians to effectively manage depression from diagnosis through treatment, follow-up, and referral when necessary.
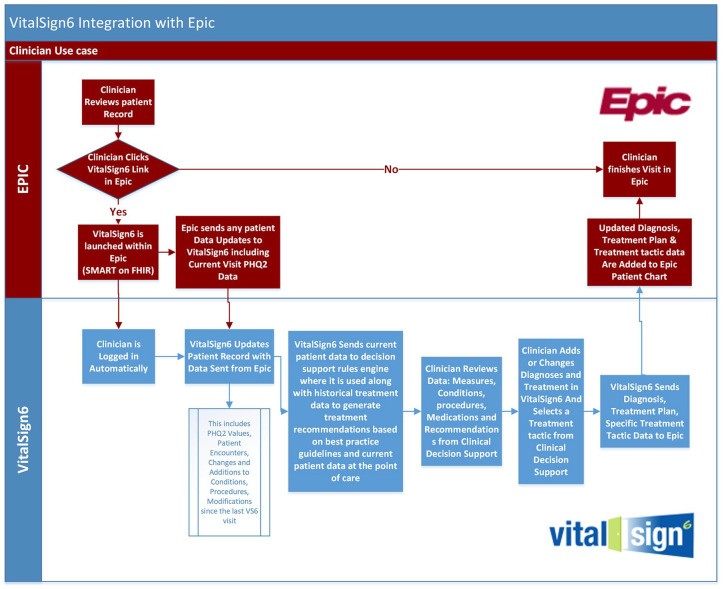
The University of Texas Southwestern Medical Center for Depression Research and Clinical Care (CDRCC) has developed an innovative MBC program called VitalSign6. This program leverages technology to seamlessly integrate depression screening and MBC into the primary care workflow. VitalSign6 incorporates an application programming interface that enables interoperability with electronic health records (EHRs), streamlining data flow and clinical decision-making.
Implementing VitalSign6 to Enhance Depression Care: A Quality Improvement Project
To demonstrate the practical impact of MBC and integrated screening tools, a quality improvement project was undertaken at the University of Texas Southwestern Medical Center (UTSW), Department of Family and Community Medicine. The project aimed to implement VitalSign6 to improve depression identification and management among adult patients in this primary care setting.
The project employed a pre-post intervention design to evaluate the effectiveness of VitalSign6 in enhancing screening rates, clinical outcomes, and provider/staff satisfaction. Key objectives included achieving high rates of depression screening using PHQ-2 and PHQ-9, administering MBC to diagnosed patients, monitoring treatment responses, and assessing user satisfaction with the VitalSign6 system and its EHR integration.
Project Methodology
The project was conducted at a primary care clinic within UTSW, involving a diverse patient population and a residency training program. Prior to implementation, comprehensive training sessions were conducted for physicians and clinic staff, covering depression education, screening protocols, MBC principles, and the use of the VitalSign6 system. VitalSign6 was integrated into the clinic’s EHR system (Epic) to facilitate seamless workflow and data management.
Patients presenting for visits were screened using PHQ-2 via tablets during check-in. Positive PHQ-2 screens or pre-existing depression history triggered further assessment with PHQ-9 using the VitalSign6 iPad application. VitalSign6 provided clinical decision support tools to assist physicians in diagnosis, treatment planning, and follow-up scheduling. Patient progress was monitored through subsequent PHQ-9 assessments at follow-up visits.
Physician and staff satisfaction with VitalSign6 was evaluated using pre- and post-implementation surveys, assessing their perceptions of depression care, comfort levels, and the usability and value of the VitalSign6 system.
Project Results: Improved Screening and Patient Outcomes
The project yielded significant improvements in depression screening rates. An impressive 95.4% of unique adult patients were screened using PHQ-2. Among those who screened positive on PHQ-2, a high percentage (89.4%) proceeded to PHQ-9 screening. Overall, a substantial proportion of patients screened with PHQ-9 were diagnosed with a depressive disorder, and the majority of those diagnosed initiated measurement-based care treatment plans.
Follow-up data revealed clinically meaningful and statistically significant reductions in patient-reported PHQ-9 scores from baseline to follow-up. Furthermore, a notable percentage of patients in follow-up achieved remission, defined as a minimal PHQ-9 score. These findings underscore the effectiveness of the VitalSign6 program in improving depression outcomes in primary care.
Image Alt Text: Graph depicting the statistically significant decrease in PHQ-9 depression scores from baseline to follow-up visits in primary care patients, indicating improved mental health through screening and treatment.
Provider and Staff Perceptions of VitalSign6
Physician and staff surveys provided valuable insights into the user experience with VitalSign6. While physicians acknowledged the importance of depression screening, post-implementation surveys surprisingly indicated a slight decrease in their perceived importance of measurement-based care. This was potentially linked to workflow disruptions and technical challenges encountered during the initial implementation phase. However, physicians and staff generally recognized the value of VitalSign6 in enhancing mental health awareness and improving depression screening within the clinic. Staff reported increased comfort levels in discussing mental health with patients following the training and implementation of VitalSign6.
Workflow integration and technical interoperability with the EHR were identified as key challenges. The simultaneous introduction of new tablet-based check-in procedures and the VitalSign6 system contributed to initial workflow slowdowns. However, the EHR integration was also recognized as a valuable aspect of VitalSign6, streamlining data access and clinical decision support.
Discussion: The Value of Depression Screening Tools in Primary Care Enhancement
The findings of this quality improvement project reinforce the critical role of depression screening tools, particularly PHQ-2 and PHQ-9, in enhancing depression care within primary care settings. The implementation of VitalSign6, incorporating these tools within a measurement-based care framework and integrated EHR system, demonstrated significant improvements in screening rates, patient outcomes, and mental health awareness.
The project highlights that addressing depression in primary care is not solely an issue of mental health access, but also a matter of effective triage and management within the primary care environment. By equipping primary care providers with evidence-based tools and clinical decision support, programs like VitalSign6 empower them to manage a large proportion of patients with depression effectively, reducing the need for specialist referrals in many cases.
Despite the positive outcomes, the project also illuminated areas for further improvement. Workflow optimization, technical enhancements to EHR interoperability, and strategies to improve patient follow-up rates are crucial for maximizing the impact and sustainability of such programs.
Conclusion: Advancing Depression Care through Integrated Screening and Measurement-Based Approaches
In conclusion, the integration of depression screening tools, such as PHQ-2 and PHQ-9, within a measurement-based care framework like VitalSign6 holds significant promise for enhancing the identification and management of depression in primary care. By leveraging technology to streamline screening, provide clinical decision support, and improve workflow integration, these approaches can contribute to better patient outcomes and a more proactive approach to mental health care within primary care settings. Continued efforts to refine implementation strategies, address workflow challenges, and improve patient engagement are essential to fully realize the potential of depression screening tools and measurement-based care in transforming primary care for mental health.
References
[References from the original article remain the same and are listed here for completeness as in the original article]