1. Introduction
Across various sectors, industries are relentlessly pursuing advancements to not only meet but exceed customer expectations, employing a diverse array of innovative methodologies. The pharmaceutical industry, a cornerstone of global well-being, plays an undeniably critical role in preserving and improving lives. This vital industry thrives on continuous innovation and the rapid adoption of cutting-edge technologies to effectively address global healthcare challenges and swiftly respond to medical emergencies, as vividly demonstrated by the recent pandemic [1]. Within the pharmaceutical domain, innovation is deeply rooted in extensive research and development across a spectrum of areas, encompassing manufacturing technologies, packaging innovations, and customer-centric marketing strategies [2]. Novel pharmaceutical advancements range from meticulously designed small drug molecules to complex biologics, with a pronounced emphasis on enhanced stability and high potency to effectively meet unmet medical needs in disease treatment. A significant area of concern and ongoing research is the assessment of potential toxicity levels associated with new drug entities. The primary objective remains the development of drug molecules that offer optimal therapeutic benefits and are ideally suited for widespread application in the healthcare sector. Despite these crucial endeavors, the pharmaceutical industry confronts numerous obstacles that necessitate further progress through technology-driven solutions to effectively address global medical and healthcare demands [3,4,5].
The persistent demand for a highly skilled workforce within the healthcare industry underscores the continuous need for comprehensive training programs for healthcare personnel, aimed at augmenting their proficiency in routine and specialized tasks. Identifying and addressing skill gaps in the workplace is a paramount undertaking for pharmaceutical organizations. It is crucial to effectively bridge these gaps through targeted remedial measures, acknowledging that delivering adequate and specialized training can itself present a considerable challenge. Recent reports indicate that approximately 41% of supply chain disruptions occurred in June 2022, highlighting supply chain vulnerabilities as a significant obstacle. Pharmaceutical industries are actively anticipating further advancements in supply chain management and innovative models to enhance resilience and address these challenges, particularly in the face of increasing cybersecurity concerns. The global outbreak of coronavirus disease 2019 (COVID-19) underscored these vulnerabilities, causing significant disruptions across worldwide operations, including ongoing clinical trials [7].
Events such as pandemics, natural disasters, fluctuating pricing, cyberattacks, logistical delays, and product-related issues significantly amplify supply chain disruptions. Transportation challenges stemming from epidemic conditions have severely impacted supply chain networks and global industries. Decision-making delays related to price updates from suppliers, often due to ambiguities regarding the application of new versus existing prices for commodities, contribute to price fluctuation delays. Emerging complexities arise from evolving cross-border trade cooperation strategies between countries, escalating criminal activity, and instability in the availability of crucial resources for operation and production. Manufacturing footprint modifications are increasingly necessary to align with evolving patient needs and stringent compliance requirements.
During the pandemic, a substantial quantity of COVID-19 vaccines became unusable due to complications in maintaining the cold chain, highlighting the critical nature of robust and secure logistical infrastructure. A primary driver of supply chain disruption stemming from delayed responses is insufficient innovation and imprecise forecasting in industrial and commercial operations. Supply chain disruptions within the pharmaceutical industry have profound ramifications on customer satisfaction, corporate reputation, and ultimately, profitability [8,9]. In today’s interconnected world, cybersecurity, much like the security considerations crucial for self-driving cars, becomes paramount. The University of Michigan (U-M) and other leading institutions are continuously releasing threat identification tools to combat digital vulnerabilities. This concept of proactive threat identification is equally critical in the pharmaceutical sector, especially as it increasingly relies on AI and digital infrastructure.
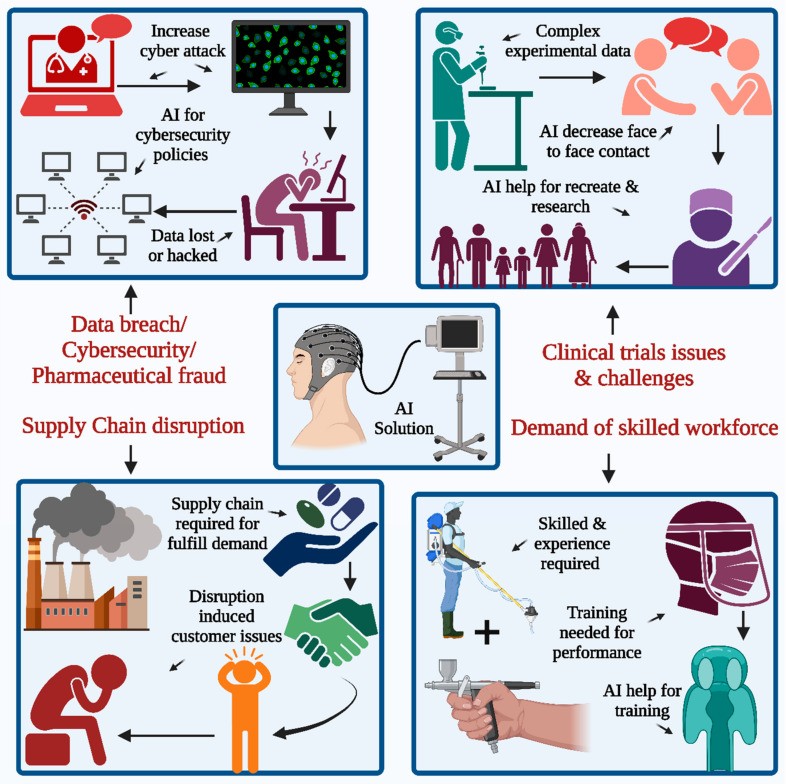
The implementation of Artificial Intelligence (AI) is poised to revolutionize supply chain operations within the pharmaceutical industry (Figure 1). AI offers the potential to consolidate decades of research and development, creating effective solutions for a wide range of supply chain challenges. Furthermore, ongoing research is exploring potential areas where AI can enhance decision-making tools for future supply chain management strategies [10,11].
Figure 1.
AI solutions for pharmaceutical industry challenges include workforce proficiency, supply chain resilience, clinical trial efficiency, and robust cybersecurity measures to combat data breaches and security threats.
The pandemic’s immediate impact is waning, yet its influence on clinical trials persists. Pharmaceutical companies are increasingly adopting advanced technologies, including AI platforms and virtual platforms, to navigate these challenges. These technologies offer valuable tools for restarting or reimagining clinical trials, minimizing the need for face-to-face interactions [12,13,14,15,16,17,18], as depicted in Figure 1. Currently, the scarcity of highly skilled workers and escalating maintenance costs pose significant hurdles. A critical challenge in leveraging technology-based solutions is the increasing threat of data breaches and cybersecurity incidents. The 21st century has witnessed a rise in cyberattacks targeting sensitive patient data, making cybersecurity a paramount concern for pharmaceutical companies. Confidential medical records and patient data are particularly vulnerable to sophisticated cyberattacks, necessitating robust protective measures. Traditional clinical trials are often plagued by data fragmentation and disconnected systems, leading to scattered data and extensive manual data transcription efforts. Innovation in trial models is lacking, resulting in rework and repetition of ongoing tasks. Patient recruitment, enrollment, monitoring, retention, and medical adherence are key areas in healthcare that require focused attention during clinical trials. Patient enrollment can be hindered by time-consuming travel to trial sites, and frequent site visits can contribute to patient attrition. AI applications in study design can optimize and streamline patient-centric design creation. AI techniques can efficiently manage the vast amounts of data generated during clinical trials, significantly reducing the need for manual data processing. Wearable devices and body sensors, integrated with AI algorithms, enable remote patient monitoring, capturing vital signs and valuable information in real-time, thereby minimizing the need for routine face-to-face interactions [19]. Just as self-driving cars require sophisticated threat identification tools for safe operation, the pharmaceutical industry needs advanced cybersecurity solutions to protect its digital assets.
Implementing effective cybersecurity measures, both within office environments and for remote workers, is now a critical imperative. Data security and robust breach prevention techniques demand special attention. Technology is also essential in addressing political fraud, which has been increasingly reported, especially during the pandemic. Proactive steps to prevent healthcare fraud, alongside fostering open internal discussions about fraudulent behaviors, are crucial for mitigating these risks.
2. Current Pharmaceutical Challenges and the Role of AI
The pharmaceutical industry is continuously engaged in research on small molecules aimed at developing superior products and enhancing customer satisfaction, driven by the numerous advantages they offer. Chemical synthesis processes are generally simpler, and the preparation of synthetic derivatives is often more economical. Consequently, the pharmaceutical sector benefits from a wide array of stable and potent small-molecule formulations. However, with the exception of treatments for rare diseases, many innovative small molecules face intense competition from generic alternatives, necessitating complex data and extensive clinical trials for successful market launch. These factors contribute to increasing economic pressures on companies to prioritize innovation. Conversely, the biomolecular drug industry is experiencing rapid growth, offsetting some of the challenges posed by small molecule competition and limitations in research dissemination. Small-molecule actions are largely determined by their conformation and reactivity [20,21,22,23,24,25,26]. Biomolecules, typically large units, primarily consist of amino acids from protein sources, along with nucleotides or ribonucleotides in the case of nucleic acids. Their stability and function are also significantly influenced by supramolecular sequences and spatial conformation [27]. Certain biomolecules, such as insulin and adalimumab, have achieved remarkable market success. Pharmacokinetic considerations for biomolecules are complex, with infusion often being the preferred and most practical administration route. Pharmacokinetic modulation and molecular stabilization are crucial aspects in nucleic acid-based research, with pharmacokinetic exposure and enhancement remaining key objectives. Technological advancements, particularly AI-driven solutions, hold promise in addressing these challenges and related issues [28,29,30,31,32,33]. While AI offers immense potential in drug delivery innovation and drug discovery, it is important to acknowledge existing limitations that necessitate human oversight and expertise to interpret complex results effectively. AI predictions are fundamentally based on datasets, yet the nuanced interpretation of results, especially in ambiguous areas, requires human intervention to arrive at sound conclusions. AI systems can encounter algorithm bias in processing information for predictions and hypothesis evaluation. Moreover, it is not uncommon for docking simulations to identify inactive molecules [34]. Therefore, critical analysis and validation by human experts remain essential for effective decision-making and cross-verification, mitigating potential system bias. Nevertheless, AI’s substantial potential for pharmaceutical applications warrants continued exploration and development to overcome current limitations and enhance its effectiveness and reliability [35]. Just as cybersecurity tools like threat identification software require constant refinement to stay ahead of evolving threats, AI in pharmaceuticals needs continuous development to maximize its benefits and minimize risks.
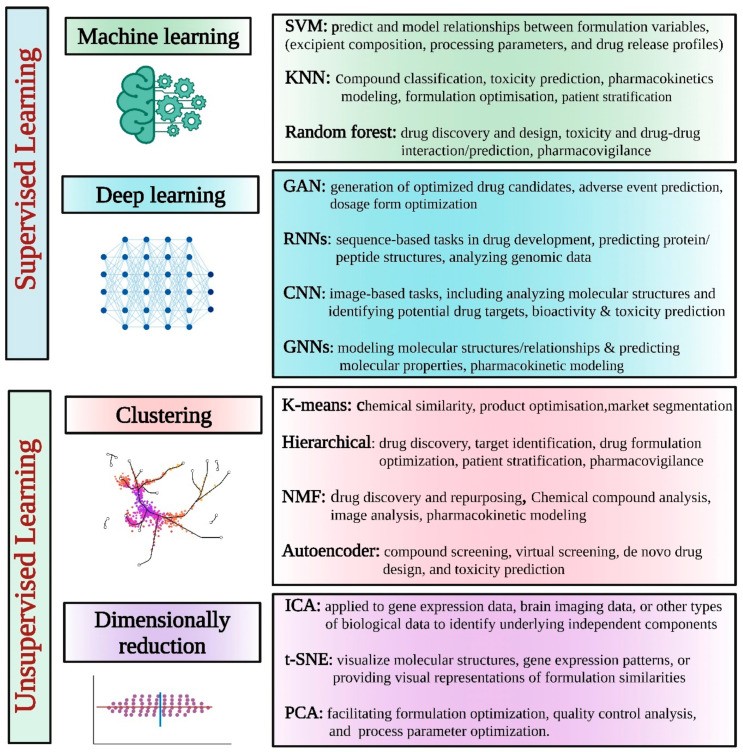
AI methodologies typically involve machine learning or its subsets, such as deep learning and natural language processing. Learning processes can be either supervised or unsupervised, with the choice of algorithm being a crucial factor. Supervised learning, a machine learning approach, utilizes known inputs (features) and outputs (labels or targets), contrasting with unsupervised learning, which deals with unknown outputs. The supervised approach focuses on predicting outputs, such as labels or targets, based on multiple inputs or features. Unsupervised classification, on the other hand, aims to create homogeneous groups based on feature similarity [36].
Various AI models have been explored to enhance different facets of pharmaceutical product development. A selection of commonly used AI models in this domain is outlined in Table 1 and Figure 2.
Figure 2.
Supervised and unsupervised AI learning models and tools applied to pharmaceutical applications.
2.1. Supervised AI Learning
Supervised learning is a machine learning paradigm where an algorithm is trained on a labeled dataset, where the desired output is already defined. By analyzing patterns and relationships within this labeled data, the algorithm learns to map input data to the correct output. This approach is widely applied in areas such as image recognition, natural language processing, and predictive modeling. Task-driven strategies in supervised learning involve setting specific goals to achieve desired outcomes from given inputs. Labeled data is used to train algorithms for tasks like data classification or outcome forecasting. The primary supervised learning tasks are classification, which predicts labels, and regression, which predicts quantities. A variety of techniques are available for supervised learning tasks, depending on the nature of the data. These techniques include Naïve Bayes, K-nearest neighbors, support vector machines, ensemble learning, random forest, linear regression, and support vector regression, among others [37]. Supervised learning has numerous applications in the pharmaceutical industry, including:
These examples illustrate the diverse applications of supervised learning in the pharmaceutical industry. Supervised learning techniques, when combined with appropriate feature selection, data preprocessing, and rigorous model evaluation, can provide valuable insights and support decision-making across various stages of pharmaceutical research, development, and manufacturing, while also considering the cybersecurity implications of handling sensitive data.
2.2. Unsupervised AI Learning
Unsupervised learning is a machine learning approach where algorithms are not provided with labeled data. Instead, they are tasked with independently identifying patterns and relationships within the data. This method is frequently used in exploratory data analysis and is valuable for uncovering hidden structures or clusters within datasets. This approach, often termed a “data-driven methodology,” aims to extract patterns, structures, or insights from unannotated data. Common unsupervised tasks include clustering, dimensionality reduction, visualization, association rule mining, and anomaly detection. Various unsupervised learning techniques are available, including clustering algorithms (e.g., hierarchical clustering, K-means, K-medoids, single linkage, complete linkage, BOTS), association learning algorithms, and feature selection and extraction techniques (e.g., Pearson correlation, principal component analysis), chosen based on the data’s characteristics [44,45]. Unsupervised learning techniques in AI are valuable in pharmaceutical applications, particularly for exploratory analysis, pattern recognition, and data visualization, as detailed below:
Unsupervised learning techniques offer valuable insights and exploratory capabilities in pharmaceutical applications. However, it is crucial to recognize that interpreting results from unsupervised learning methods often requires domain expertise and further validation to ensure the reliability and actionability of findings, especially when considering the cybersecurity aspects of data handling and analysis.
Table 1.
Top 10 commonly used AI models in the pharmaceutical industry.
| AI/Machine Learning Models | Description/Usage | References |
|---|---|---|
| Generative Adversarial Networks (GANs) | GANs are widely used in drug product development to generate novel chemical structures and optimize their properties. GANs consist of a generator network that creates new molecules and a discriminator network that evaluates their quality, leading to the generation of structurally diverse and functionally optimized drug candidates. | [52] |
| Recurrent Neural Networks (RNNs) | RNNs are commonly employed for sequence-based tasks in drug development, such as predicting protein structures, analyzing genomic data, and designing peptide sequences. They capture sequential dependencies and can generate new sequences based on learned patterns. | [53] |
| Convolutional Neural Networks (CNNs) | CNNs are effective in image-based tasks, including analyzing molecular structures and identifying potential drug targets. They can extract relevant features from molecular images and aid in drug design and target identification | [54] |
| Long Short-Term Memory Networks (LSTMs) | LSTMs are a type of RNN that excel in modeling and predicting temporal dependencies. They have been used in pharmacokinetics and pharmacodynamics studies to predict drug concentration-time profiles and evaluate drug efficacy. | [55] |
| Transformer Models | Transformer models, such as the popular BERT (Bidirectional Encoder Representations from Transformers), have been employed in natural language processing tasks in the pharmaceutical domain. They can extract useful information from the scientific literature, patent databases, and clinical trial data, enabling researchers to make informed decisions in drug development. | [56] |
| Reinforcement Learning (RL) | RL techniques have been applied to optimize drug dosing strategies and develop personalized treatment plans. RL algorithms learn from interactions with the environment to make sequential decisions, aiding in dose optimization, and improving patient outcomes. | [57] |
| Bayesian Models | Bayesian models, such as Bayesian networks and Gaussian processes, are employed for uncertainty quantification and decision-making in drug development. They enable researchers to make probabilistic predictions, assess risks, and optimize experimental designs. | [58,59] |
| Deep Q-Networks (DQNs) | DQNs, a combination of deep learning and reinforcement learning, have been used to optimize drug discovery processes by predicting the activity of compounds and suggesting high-potential candidates for further experimentation. | [60,61] |
| Autoencoders | Autoencoders are unsupervised learning models used for dimensionality reduction and feature extraction in drug development. They can capture essential characteristics of molecules and assist in compound screening and virtual screening. | [62,63] |
| Graph Neural Networks (GNNs) | GNNs are designed to process graph-structured data, making them suitable for drug discovery tasks that involve molecular structures. They can model molecular graphs, predict properties, and aid in virtual screening and de novo drug design. | [64,65] |
3. AI for Drug Discovery
AI has fundamentally transformed drug research and discovery in numerous significant ways, enhancing efficiency and accelerating timelines. Key contributions of AI in this domain include:
3.1. Target Identification
AI systems possess the capability to analyze diverse data types, including genetic, proteomic, and clinical data, to pinpoint potential therapeutic targets. By identifying disease-associated targets and relevant molecular pathways, AI aids in the rational design of medications capable of modulating specific biological processes. This is analogous to how cybersecurity threat identification tools pinpoint vulnerabilities within complex systems.
3.2. Virtual Screening
AI facilitates the efficient screening of extensive chemical libraries to identify drug candidates with a high probability of binding to specific targets. By simulating chemical interactions and predicting binding affinities, AI helps researchers prioritize and select compounds for experimental testing, conserving valuable time and resources. This virtual approach mirrors the proactive nature of cybersecurity threat identification tools that scan for potential risks before they materialize.
3.3. Structure-Activity Relationship (SAR) Modeling
AI models can establish correlations between the chemical structure of compounds and their biological activity. This enables researchers to optimize drug candidates by designing molecules with desirable characteristics, such as enhanced potency, selectivity, and favorable pharmacokinetic profiles. Similar to how cybersecurity tools analyze network traffic patterns to identify malicious activity, SAR modeling uses data patterns to optimize drug design.
3.4. De Novo Drug Design
Utilizing reinforcement learning and generative models, AI algorithms can propose entirely novel drug-like chemical structures. By learning from vast chemical libraries and experimental data, AI expands the explored chemical space and facilitates the development of innovative drug candidates. This innovative design process parallels the continuous evolution of cybersecurity threat identification tools to counter new forms of digital attacks.
3.5. Optimization of Drug Candidates
AI algorithms can analyze and optimize drug candidates by considering multiple factors, including efficacy, safety, and pharmacokinetics. This assists researchers in fine-tuning therapeutic molecules to maximize their effectiveness while minimizing potential side effects. Just as cybersecurity systems are optimized to balance protection with system performance, AI optimizes drug candidates for therapeutic effectiveness and safety.
3.6. Drug Repurposing
AI techniques can analyze large-scale biomedical datasets to identify existing drugs that may possess therapeutic potential for different diseases. By repurposing approved drugs for new indications, AI accelerates the drug discovery process and significantly reduces development costs. This efficient repurposing strategy is similar to leveraging existing cybersecurity infrastructure to address new threats.
3.7. Toxicity Prediction
AI systems can predict drug toxicity by analyzing the chemical structure and characteristics of compounds. Machine learning algorithms trained on comprehensive toxicology databases can anticipate harmful effects or identify hazardous structural properties. This helps researchers prioritize safer chemicals and mitigate potential adverse responses in clinical trials. Proactive toxicity prediction parallels the proactive threat identification in cybersecurity, aiming to prevent harmful outcomes.
Overall, AI-driven approaches in drug research and development offer the potential to streamline and expedite the identification, optimization, and design of novel therapeutic candidates, ultimately leading to more efficient and effective medications [66]. The integration of cybersecurity measures into AI-driven drug discovery is crucial to protect sensitive research data and intellectual property.
For instance, in silico target fishing technology (TF) is utilized in pharmaceuticals for biological target prediction based on chemical structure, drawing on information available in chemical databases in a biologically annotated format. Alongside TF, other methods such as data mining and chemical structure docking are employed to explore mechanisms of action and target class information, essential for effective planning. Target fishing techniques, enhanced by machine learning and cheminformatics tools, are invaluable in drug discovery, providing detailed insights into complex structures and aiding in the design of novel drug ingredients for complex disease treatments. Traditional drug discovery methods can be costly and complex, involving intricate steps like target protein selection and mechanism of action elucidation. TF accelerates this process and reduces experimental costs. Reference molecules with 3D descriptors are used for ligand-target prediction. TF has been applied to identify the high binding affinity of diethylstilbestrol and is widely used in phytopharmacology studies and similarity assessments. It is a computational and proteomics-based method that ranks data points based on similarity in data fusion and drug targets. TF also aids in predicting potential toxicities for ligand-based drug discovery approaches. Key aspects of drug development and discovery, such as novel target identification, phytopharmacological profile prediction, and adverse effect prediction, are explored using TF. Bioactive compound similarity is applied to identify targets for unrecognized compounds. Drugs successfully characterized using TF include loperamide, emetine, and methadone, with identified targets including muscarinic, adrenergic, and neurokinin receptors [2,67,68,69,70,71,72,73,74,75]. The security and integrity of the data used in these AI-driven tools are paramount, mirroring the need for robust cybersecurity in all digital systems.
The field of drug discovery has witnessed significant advancements with the integration of AI models and tools. Table 2 lists some popular AI model tools used in drug discovery. This is just a selection, as the field is rapidly evolving with continuous development of new tools and models to accelerate drug discovery processes.
Table 2.
Popular AI model tools used for drug discovery.
| AI Model Tools | Summary |
|---|---|
| DeepChem | An open-source library that provides a wide range of tools and models for drug discovery, including deep learning models for molecular property prediction, virtual screening, and generative chemistry. |
| RDKit | A widely used open-source cheminformatics library that offers various functionalities for molecule handling, substructure searching, and descriptor calculation. It can be integrated with machine learning frameworks for drug discovery applications. |
| ChemBERTa | A language model specifically designed for drug discovery tasks. It is based on the Transformer architecture and is pretrained on a large corpus of the chemical and biomedical literature, allowing it to generate molecular structures, predict properties, and assist in lead optimization. |
| GraphConv | A deep learning model architecture that operates on molecular graphs. It has been successful in predicting molecular properties, such as bioactivity and toxicity, by leveraging the structural information encoded in the graph representation of molecules. |
| AutoDock Vina | A popular docking software that uses machine learning techniques to predict the binding affinity between small molecules and protein targets. It can assist in virtual screening and lead optimization for drug discovery. |
| SMILES Transformer | A deep learning model that takes Simplified Molecular Input Line Entry System (SMILES) strings as input and generates molecular structures. It can be used for de novo drug design and lead optimization. |
| Schrödinger Suite | A comprehensive software package for drug discovery that incorporates various AI-driven tools. It includes modules for molecular modeling, virtual screening, ligand-based and structure-based drug design, and predictive modeling. |
| IBM RXN for Chemistry | An AI model designed to predict chemical reactions. It utilizes deep learning algorithms and large reaction datasets to generate potential reaction outcomes, aiding in the discovery of new synthetic routes and compound synthesis. |
| scape-DB | scape-DB (Extraction of Chemical and Physical Properties from the Literature-DrugBank) is a database that combines natural language processing and machine learning to extract chemical and biological data from the scientific literature. It provides valuable information for drug discovery research. |
| GENTRL(Generative Tensorial Reinforcement Learning) | A deep learning model that combines reinforcement learning with generative chemistry to design novel molecules with desired properties. It has been used for de novo drug design and optimization. |
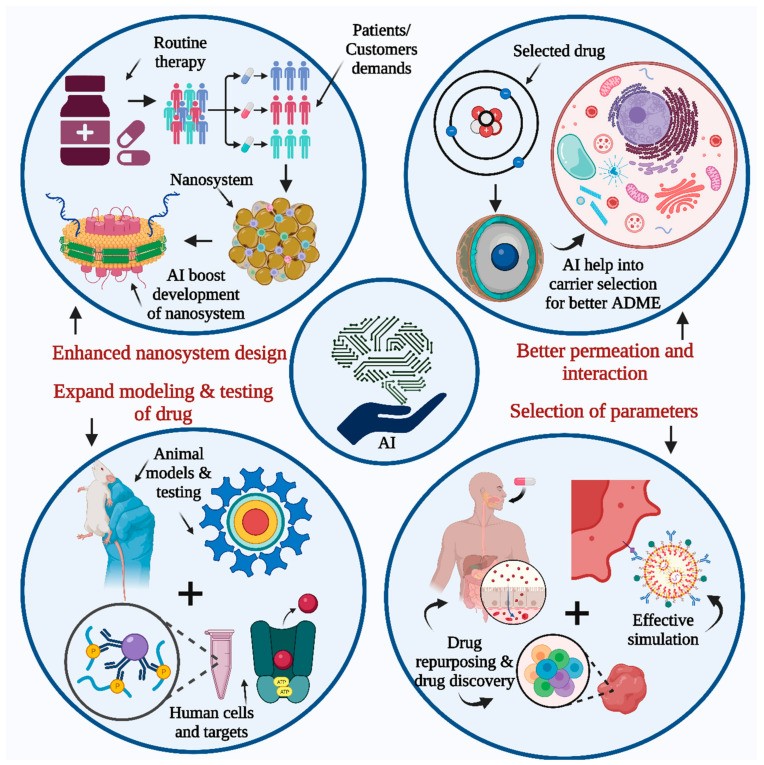
4. AI Tool Application in Dosage Form Designs
The human body system is compartmentalized to understand drug delivery impact, further simplified based on biological membranes. Physicochemical barriers are crucial for these compartments and depend on the drug delivery mode. Permeation rate, determined by administration route, is a critical factor for efficient drug delivery system monitoring. Orally administered drugs must permeate through the intestinal or gastric epithelium after entering the gastric environment, a vital step for bloodstream distribution. Distribution delivers the drug to the target site, which can be tissue or specific cellular components [76,77,78,79,80]. Intracellular molecules can also be drug targets. Drug permeation through biological barriers is primarily passive or active. Passive diffusion depends on drug molecular features. In silico models predict drug distribution computationally, but results may differ from actual drug distribution studies. Drug-biological component interaction and drug availability in biological environments significantly affect drug fate, governed by drug molecular features. Passive permeation is inefficient for many bioactive entities and small molecules, necessitating specific drug delivery systems. Active permeation, driven by membrane transport, depends on complex biological interactions. This complexity requires exploration using computational and systematic modeling approaches. Newer computational models study pharmacokinetic parameters of drug delivery systems. A major challenge in pharmaceutical R&D is the predictability of preclinical models, based on selected parameters, also applicable to complex in silico models. Drug-membrane interactions, better analyzed in modeled environments (Figure 3), can be effectively studied using AI [81,82,83]. AI provides sophisticated technology for analyzing multilayer data, enhancing research unit understanding. Systematic modeling with parameter evaluation involves simulation, scoring, and refinement at each research step for optimal outcomes. AI can automate these functions for improved data prediction and refinement, requiring a thorough understanding of drug-biological interactions, facilitated by system biology databases, for effective AI training in biological environments. Pharmacokinetic studies benefit from AI technologies like artificial neural networks and AI-provided databases (chemical, genomic, phenotypic) for better drug interaction understanding and complex molecular unit role studies. Methods also assess drug delivery system impact on drug pharmacokinetics, disposition, and toxicity. New drug delivery system approaches involve designing quality and critical attributes and studying their impacts in experimental trials before actual experiments. Just as cybersecurity systems require robust design and testing to prevent vulnerabilities, AI-driven dosage form designs must be rigorously validated.
Figure 3.
AI’s contribution to drug development and research includes enhancing nanosystem design, improving drug testing modeling, and increasing accuracy in parameter and factor selection for drug design, discovery, and repurposing. It also aids in understanding membrane interaction mechanisms with modeled human environments by studying drug permeation, simulation, and human cell targets.
AI’s benefits include information collection from multiple sources, guiding drug delivery system selection for anticipated results. Molecular, patient, and pharmacokinetic data evaluation are part of complex data analysis for selecting the best active pharmaceutical against patient diseases. Passive AI identifies molecular entity features for comparison with known molecules. Effective treatment relies on accurate drug delivery system selection, facilitated by AI. The threat identification capabilities of AI can be applied to analyze vast datasets of dosage form performance to optimize design and predict potential issues.
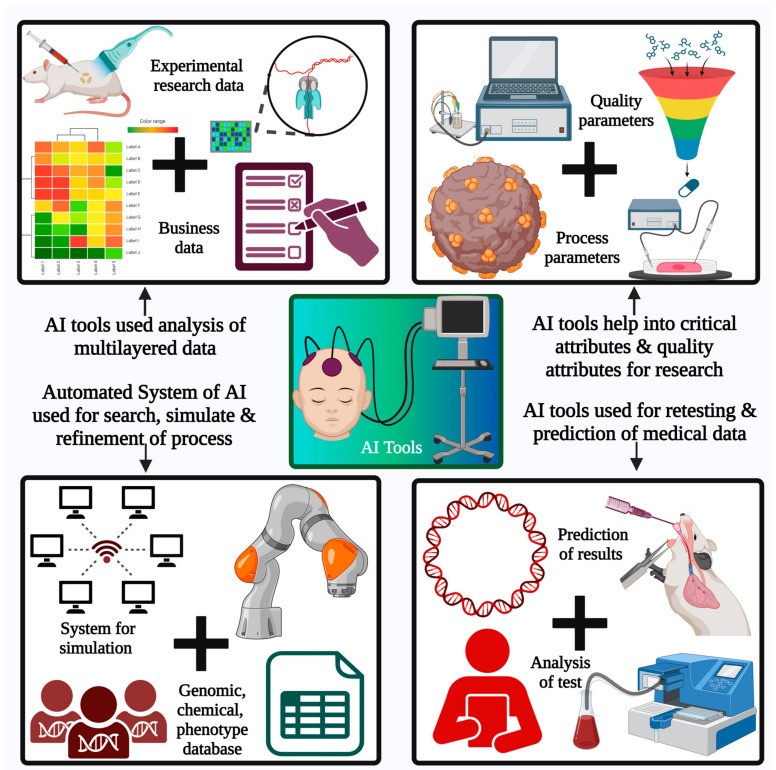
AI is also valuable for drug discovery and repurposing, addressing new disease applications for existing therapeutics. Patient and disease conditions are major factors influencing formulation, pharmacokinetics, and drug development. A key challenge in AI application for delivery system development is the availability of detailed databases for unbiased model and parameter evaluation. AI uses current knowledge for future applications, handling large data quantities for rational product design (Figure 4). Vigorous knowledge database codification with self-supervised experimental results and proper parameter recording is crucial [84,85,86,87,88,89,90].
Figure 4.
AI tool applications in the pharma sector include multilayered data analysis. Automated AI systems perform effective searches, simulations, and data and process refinements in research and product development. System biology, chemical, genomic, phenotypic databases, and AI bots explore drug models, release, activity predictions, and recommend effective drug delivery systems.
5. AI for Drug Delivery
Integrating AI and big data in pharmaceutics has led to computational pharmaceutics, enhancing drug delivery through multiscale modeling. Computational pharmaceutics uses AI algorithms and machine learning to analyze large datasets and predict drug behavior (Table 3). Simulating drug formulation and delivery allows researchers to evaluate scenarios and optimize systems without extensive trial-and-error, accelerating development, reducing costs, and increasing productivity. Computational pharmaceutics models drug delivery systems at scales from molecular interactions to macroscopic behavior. AI analyzes complex relationships between drug properties, formulation components, and physiological factors to predict drug behavior at each scale, providing comprehensive understanding and aiding efficient drug delivery system design. It predicts drug physicochemical properties, in vitro release profiles, and stability, also assessing in vivo pharmacokinetic parameters, drug distribution, and in vivo-in vitro correlation. Using appropriate AI tools, researchers can identify potential risks and challenges early, enabling proactive modifications and minimizing unforeseen outcomes [91,92]. Similar to how cybersecurity tools perform risk assessments to identify and mitigate potential digital threats, AI in drug delivery identifies and mitigates risks in formulation and delivery systems.
5.1. AI for Oral Solid Dosage Form Development
AI, utilizing advanced tools and software for human-like capabilities, has benefited sectors like pharmaceuticals, especially in product development. Technological innovations save time, money, and resources in manufacturing and supply chain distribution. AI improves understanding of process parameter impacts on formulation and manufacturing.
Run Han et al. used machine learning to predict solid dispersion stability for six months. Hanlu Gao et al. applied machine learning for solid dispersion dissolution studies, using a random forest algorithm to classify dissolution profiles (spring and parachute types). It also maintained supersaturation with 85% accuracy and 86% sensitivity, predicting time-dependent drug release with a random forest regression model [93].
Solid dosage forms, particularly tablets, dominate the pharmaceutical market. Tablet preparation involves numerous factors. AI can optimize formulation and study desired attributes. AI is expected to automate obligations using algorithms and technologies. Regulatory authorities face challenges in redefining policies for current good manufacturing practice (cGMP). AI technologies like artificial neural networks (ANNs), fuzzy logics, neural networks, and genetic algorithms are used for solid dosage form development and input-output understanding. ANNs improve prediction abilities for solid dosage forms, while genetic algorithms predict results from input parameters [94]. The threat identification capabilities of AI can be used to detect anomalies and predict potential quality issues in solid dosage form manufacturing.
Table 3.
List of commonly explored AI models in pharmaceutical product development.
| AI/Machine Learning Models | Description/Usage | References |
|---|---|---|
| Genetic Algorithms | Genetic algorithms are optimization techniques inspired by the principles of natural selection and genetics. They can be applied to optimize formulation compositions, drug release profiles, and process parameters to achieve desired dosage form characteristics. | [95] |
| Artificial Neural Networks (ANNs) | ANNs have been employed to model and optimize drug release kinetics from different dosage forms. They can assist in determining optimal formulations and predict the release behavior of active pharmaceutical ingredients (APIs) under various conditions. | [96] |
| Support Vector Machines (SVMs) | SVMs have been used in dosage form optimization to predict and model relationships between formulation variables, such as excipient composition, processing parameters, and drug release profiles. They aid in optimizing formulation design space. | [97] |
| Particle Swarm Optimization (PSO) | PSO is a population-based optimization algorithm that can be used for dosage form optimization. It has been applied to optimize particle size distribution, dissolution profiles, and other formulation parameters. | [98] |
| Artificial Intelligence-based Expert Systems | Expert systems utilize AI techniques, including rule-based systems and fuzzy logic, to simulate the decision-making process of human experts. They can be applied to dosage form optimization by considering multiple formulation and process variables. | [99] |
| Monte Carlo Simulation | Monte Carlo simulation methods have been used to optimize drug product performance by considering uncertainties and variability in formulation and process parameters. They aid in robust formulation and process design. | [100] |
| Computational Fluid Dynamics (CFD) | CFD simulations enable the optimization of fluid flow and mixing within dosage form manufacturing processes, such as granulation, coating, and drying. They help in designing efficient and uniform processes. | [101,102] |
| Response Surface Methodology (RSM) | RSM is a statistical technique that helps optimize dosage form formulations by modeling and analyzing the relationship between multiple variables and their effect on formulation responses. It aids in understanding and optimizing formulation parameters. | [103,104,105] |
| Artificial Neural Network–Genetic Algorithm (ANN-GA) Hybrid Models | Hybrid models combining ANN and GA techniques have been used for dosage form optimization. They can efficiently search the formulation space to identify optimal solutions and predict formulation characteristics. | |
| Multivariate Analysis Techniques | Multivariate analysis methods, such as principal component analysis (PCA) and partial least squares (PLS), have been employed in dosage form optimization. They aid in identifying critical formulation variables, reducing dimensionality, and optimizing formulation performance. | [106,107,108] |
Tablets, a dominant solid dosage form, constitute a significant market share in drug delivery. Their production involves active pharmaceutical ingredients and excipients, compressed or molded into desired shapes and sizes. Excipients are crucial for tablet properties like disintegration, dissolution, and drug release, tailored by formulators to patient needs. Excipients also aid manufacturing, such as glidants and lubricants. AI can predict drug release in systemic delivery and study critical processing parameters in tablet manufacturing to ensure consistent quality control and detect tablet defects [109,110].
5.1.1. Prediction of Drug Release through Formulations
Predicting drug release enhances quality control. In vivo and in vitro drug release studies are fundamental technologies in product development. Drug release from oral solid dosage forms is influenced by critical material attributes and processing parameters, including compaction pressure, tablet geometry, and drug loading. Spectrophotometric analysis and extensive testing are common in drug release studies.
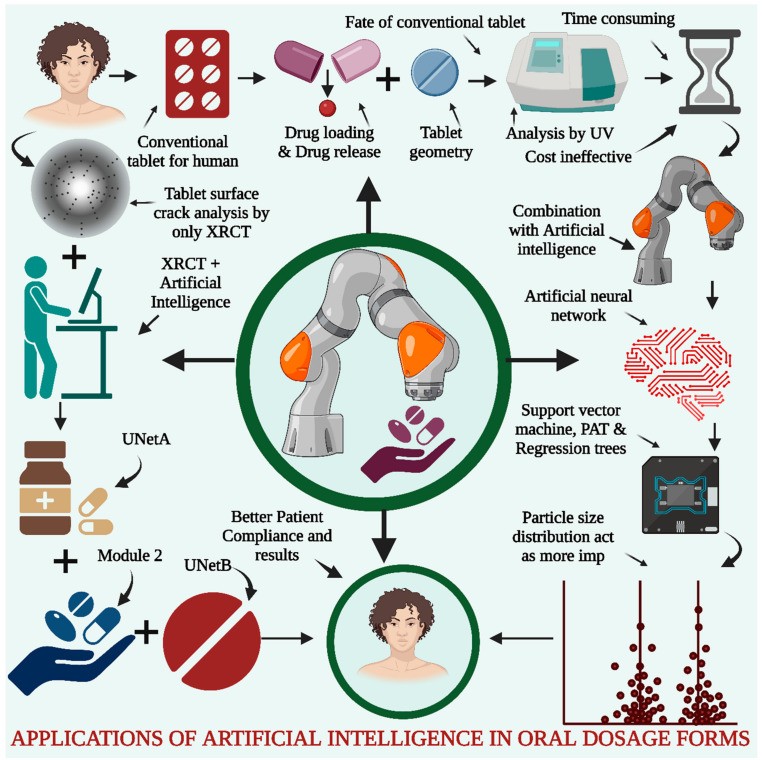
Optimizing drug release to meet formulator requirements involves repetitive testing and batch preparation, making it time-consuming [111]. AI in drug formulation can predict drug release, reducing required runs and costs in pilot and production scales. AI can predict drug and dissolution profiles and disintegration time for optimal batch selection. Researchers have used AI algorithms, specifically ANNs, to predict dissolution profiles in hydrophilic matrix sustained-release tablets. Support vector machines (SVMs) and regression analysis are also used for data analysis and dissolution profile prediction. Data for modeling drug release is obtained using process analytical technology (PAT) and critical material attributes. Particle size distribution is a critical variable in model prediction. ANN models are used for accurate model identification based on evaluation metrics (Figure 5) [112,113]. Just as cybersecurity systems need predictive capabilities to anticipate and prevent threats, AI in drug formulation predicts drug release profiles for quality control.
Figure 5.
AI for Oral Dosage Forms. Conventional tablet analysis, including drug release, loading, geometry, and hardness studies, uses in-process quality control tests and ultraviolet spectrophotometry, which are time-consuming and costly. Combining traditional techniques with AI, such as ANN, SVM, PAT, and regression trees, addresses these issues. Data analysis and drug release predictions indicate particle size distribution as crucial. XRCT with AI analyzes defective tablet surface cracks using three modules for feature distinction in healthcare applications.
5.1.2. Application of AI for 3D-Printed Dosage Forms
AI application in 3D-printed dosage forms has revolutionized pharmaceutical manufacturing, enabling personalized medicine and enhanced drug delivery systems. AI algorithms optimize 3D-printed dosage form design and formulation based on patient-specific factors like age, weight, and medical history, leading to tailored therapies. Machine learning and computational modeling allow AI to analyze large datasets and simulate 3D-printed dosage form behavior, enabling rapid prototyping and optimization of drug release profiles, dosages, and geometries. AI also predicts and overcomes manufacturing challenges, optimizing printing parameters and ensuring quality control. AI-driven feedback systems continuously improve the 3D-printing process by learning from real-time data, enhancing accuracy, reproducibility, and scalability. AI in 3D-printed dosage forms holds significant potential for advancing personalized medicine and improving patient outcomes [114,115]. Just as cybersecurity systems adapt and learn to counter evolving threats, AI in 3D printing continuously improves dosage form design and manufacturing.
3D-printed tablets are prepared using fused-filament fabrication, binder jetting, laser sintering, and pressure microsyringes. Processing parameters like nozzle and platform temperature and printing speed are critical. Obeid et al. demonstrated the impact of processing parameters on 3D-printed diazepam tablets and their drug release using an ANN model, exploring infill pattern, density, and other variables for drug dissolution. Self-organizing maps evaluated variable interactions. Modeling studies highlighted infill density, surface area, and volume ratio as crucial factors. Extensive testing and ANN modeling with validation resulted in higher dissolution [116,117].
5.1.3. Application of AI for the Detection of Tablet Defects
AI application in tablet defect detection has revolutionized quality control in pharmaceutical manufacturing. AI algorithms and computer vision analyze tablet images for automated and efficient defect detection, including cracks, chips, discoloration, and shape/size variations. AI models trained on large labeled image datasets accurately classify and identify defect types with high precision and recall. Conventional methods like X-ray computed tomography for internal tablet structure analysis are time-consuming, hindering rapid production. Deep learning with X-ray tomography improves tablet defect detection. Ma et al. explored neural networks for tablet defect detection using X-ray tomography image analysis. They manufactured tablet batches with microcrystalline cellulose and mannitol and used image augmentation strategies. Three models were used: UNetA for distinguishing tablet characteristics from bottles, Module 2 for individual tablet identification, and UNetB for internal crack analysis. UNet networks improve tablet defect checking accuracy, reducing time, costs, and workload [118,119]. AI-powered defect detection enhances speed and accuracy, reduces manual inspection dependence, minimizes human error, and provides real-time monitoring for prompt defect detection, preventing faulty tablet release, improving product quality, and ensuring pharmaceutical product safety and efficacy. Similar to how cybersecurity threat identification tools automatically scan for and identify security vulnerabilities, AI in tablet manufacturing automatically detects and identifies defects, ensuring product quality and safety.
5.1.4. AI for the Prediction of Physicochemical Stability
AI has emerged as a powerful tool for predicting oral dosage form physicochemical stability in pharmaceutical research. AI leverages machine learning algorithms and computational models to analyze large datasets, including drug properties, formulation parameters, and environmental conditions. AI models assess drug degradation, excipient interactions, and environmental effects on formulation stability. These predictive capabilities allow researchers to optimize formulations, identify potential stability issues early, and enhance the shelf life and efficacy of oral dosage forms. AI integration in stability prediction improves drug development efficiency and cost-effectiveness, ensuring safe and effective medication delivery. Researchers have studied machine learning for solid dispersion determination using various algorithms. Han et al. explored machine learning for solid dispersion prediction using ANN, K-nearest neighbor (KNN), and light gradient boosting machine (LightGBM) algorithms, along with SVM. KNN, a nonparametric supervised learning classifier, classifies or predicts groupings and individual data points [120]. LightGBM, a free, open-source distributed gradient boosting framework, is used for ranking, classification, and machine learning tasks. In this study, approximately fifty drug molecules with 646 physical stability data points from public databases were used for training. Database generation involved molecular representations and descriptors like molecular weight and hydrogen bond acceptor count, melting point, and heavy atom count. Accelerated stability studies for three months evaluated model performance in physical stability prediction, achieving 82% overall accuracy [121,122]. Just as cybersecurity systems predict and prevent security breaches, AI predicts physicochemical stability to ensure drug product integrity and efficacy over time.
5.1.5. Contribution of AI to Dissolution Rate Predictions
Drug dissolution rate, crucial for bioavailability and therapeutic effectiveness, is significantly aided by AI predictions, optimizing drug formulations and dosage forms. Analyzing vast experimental data, AI models identify key physicochemical properties and molecular features influencing dissolution. Machine learning algorithms learn complex patterns between drug properties and dissolution rates, enabling accurate predictions. AI insights into dissolution behavior facilitate the design of more effective drug delivery systems and optimal formulation strategies for enhanced drug solubility and absorption. AI-powered dissolution rate prediction empowers pharmaceutical scientists with valuable tools to accelerate drug development, optimize formulations, and improve patient outcomes [97]. Similar to how cybersecurity threat intelligence predicts potential cyberattacks, AI predicts drug dissolution rates, enabling proactive formulation optimization.
Researchers have studied dissolution profiles, documenting rapid dissolution and supersaturation of some drugs. Amorphous drug recrystallization and precipitation are critical factors. Solid dispersions can prevent precipitation with excipients. Dong et al. explored AI for predicting dissolution and dissolution rate for at least 50 APIs and 25 polymers, using algorithms like SVM, LightGBM, and extreme gradient boosting (XGBoost) [123]. XGBoost, a scalable machine learning library with a distributed gradient-boosted decision tree, helps predict problems with unstructured data like images and texts. ANNs outperformed other algorithms/frameworks. Molecular computational software was used for API and polymer descriptors. Input variables included temperature, drug loading, and volume, with dissolution as binary output (precipitation or supersaturation). Dissolution rate was the research output, resulting in greater prediction accuracy for API and polymer dissolution profiles [124,125].
5.2. AI for Nanomedicine
AI, with its data analysis, pattern recognition, and optimization capabilities, enhances nanomedicine research, accelerating nanoscale intervention development, improving diagnostics, drug delivery, and personalized medicine. AI in nanomedicine has significant potential to revolutionize healthcare through precise and targeted therapeutic approaches at the nanoscale [126]. Nanoparticles are used for targeted drug delivery, imaging, and sensing. AI algorithms aid in nanoparticle design and optimization by predicting physicochemical properties, stability, and efficacy, helping develop nanoparticles with desired characteristics for specific applications. Nanomedicines effectively deliver drugs or drug combinations, especially for cancer treatment, based on drug synergy, with impactful inputs like drug and dose selection and stimuli-responsive material selection. Deep learning algorithms for melanoma have shown high accuracy in patient care and diagnostics [127,128]. Just as cybersecurity tools are essential for protecting sensitive data in digital systems, AI is crucial for designing and optimizing nanomedicine for targeted and safe drug delivery.
AI algorithms model nanoscale material behavior and interactions within biological systems, predicting nanoparticle behavior, drug release kinetics, and potential toxicity, facilitating safe and effective nanomedicine formulations. AI can be used in nanosensors and biosensors for real-time biomarker, drug level, and disease progression monitoring, providing continuous feedback for timely interventions and personalized treatment adjustments [129].
AI-based databases aid nanocarrier scale-up using automation. AI is also used in nanocarrier drug delivery systems for optimization and drug compatibility testing using computational approaches to evaluate drug loading, formulation stability, and drug retention. AI enhances therapeutic nanocarriers for specific tumor cell types. Yuan He et al. used machine learning to predict nanocrystals prepared by high-pressure homogenization and wet ball milling. Computational techniques like Monte Carlo simulations, molecular dynamics, and theoretical techniques reduce experimental repetition. Simulation techniques quantify critical experiments. AI creates database repositories for nanocarriers, determining 3D structures and investigating physical and chemical properties with structural nanobiology collaboration. Such repositories are essential for studying nanocarrier structure relationships with toxicological, physical, and biological data [130,131,132,133,134,135,136,137]. Lutz Nuhn found AI helpful in revealing heterogeneous vascular permeability for nanoparticle-based drug delivery systems using single blood vessel analysis, aiding protein nanoparticle drug delivery system design for active transendothelial permeability into tumors [138]. Zhoumeng Lin et al. used AI with PBPK modeling to study cancer medicine effectively and understand causes of low nanoparticle tumor delivery efficacy [139].
5.3. AI Application for Parenteral, Transdermal and Mucosal Route Products
AI aids in developing and manufacturing injectables, biologics, and complex formulations. Predicting physicochemical parameters of complex drug formulations using AI systems can enhance formulation development. AI models optimize pH, solubility, stability, and viscosity by analyzing formulation components, excipients, and manufacturing processes, helping create stable parenteral formulations. AI optimizes parenteral product production for quality, efficiency, and variability, identifying process factors affecting product qualities and suggesting modifications by analyzing real-time process data, increasing product consistency, reducing batch failures, and improving manufacturing productivity. AI algorithms find trends and product quality variations in large datasets from analytical tests, helping identify and fix quality concerns early, ensuring high-quality products. AI models can predict contamination, stability, and regulatory deviations using historical data and process factors. AI-based monitoring systems analyze key process parameters in real-time during parenteral product manufacturing, identifying abnormalities, forecasting deviations, and enabling quick action by combining data from sensors, instruments, and process controls, maintaining product quality and minimizing noncompliance. AI optimizes maintenance procedures for complex parenteral product manufacturing equipment, forecasting equipment failure or deterioration and scheduling proactive maintenance by analyzing sensor data, equipment performance history, and maintenance records, saving downtime, boosting output, and cutting maintenance costs. AI can help ensure parenteral and complex biological product regulatory compliance, analyzing compliance data, detecting potential noncompliance concerns, and providing process improvement ideas by analyzing process data and product properties, aiding GMP and regulatory compliance [140]. Just as cybersecurity monitoring systems detect anomalies and potential threats in network traffic, AI monitoring systems detect anomalies and potential quality or compliance issues in parenteral product manufacturing.
For example, AI is used in particle inspection to check for swimming, sinking, or sticking particles in containers. Optical setups, strategies, algorithms, and inspections are recommended for particle inspection. Particle tracking algorithms and image subtraction analyze floating particles. Liquid movement inside containers allows recording of particle behavior with high-resolution images, and AI traces particle movement direction. Deep learning algorithms isolate particles. Bubble formation, a common parenteral batch flaw, requires distinguishing between particles and bubbles, addressed by AI-based image processing algorithms for visual inspection. Camera-based AI applications include surface crack detection using Surface Qualify 7500, analyzing millions of data points per second using graphical processing subunits [127,128,140,141,142]. AI data analysis, pattern recognition, and predictive modeling enable manufacturers to optimize product performance, reduce manufacturing hazards, and provide safe and effective parenteral and technologically advanced pharmaceutical products.
Bannigan et al. highlight machine learning (ML) technologies in pharmaceutical and materials science, demonstrating ML’s ability to predict in vitro drug release from long-acting injectables (LAIs), accelerating innovative drug delivery technology development. ML model interpretability is emphasized. Tree-based models like LGBM show promise in reducing LAI formulation development time and cost, providing a proof-of-concept for ML in drug formulation and inspiring advanced and tailored ML approaches [143,144].
Conventional trial-and-error methods in formulating ocular, transdermal, pulmonary, and mucosal drug delivery systems are inefficient for complex formulations due to a lack of in-depth understanding. Computational pharmaceutics advancements, especially machine learning and multiscale simulations, offer new possibilities. Molecular simulations, mathematical modeling, and PK/PD modeling for these routes enhance product development efficiency. In silico modeling and simulations provide detailed insights and facilitate rational formulation design. Integrating in silico methodologies, addressing data challenges, and fostering interdisciplinary collaborations can lead to more efficient and objective drug formulation design in Pharma 4.0 [145,146,147,148].
5.4. AI Tools for Biologics Product Development
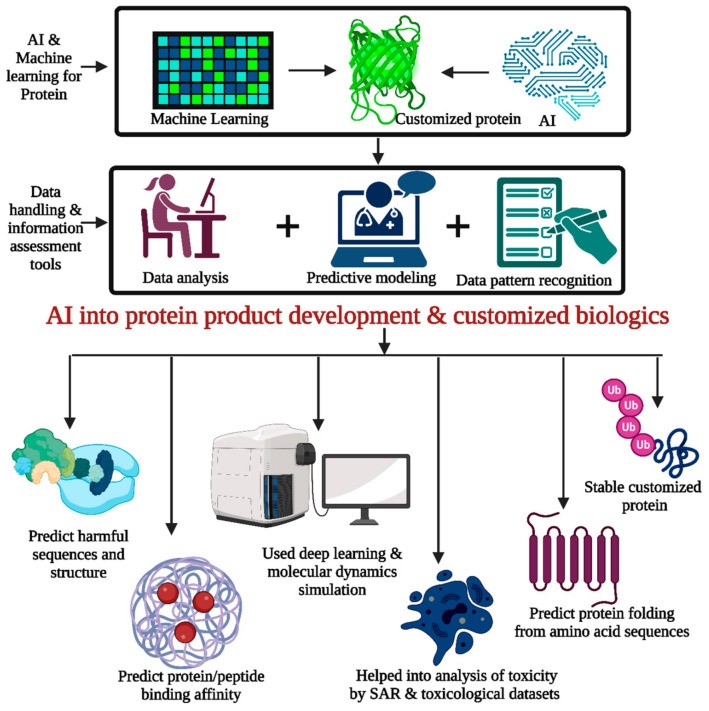
AI assists in creating novel proteins, peptides, nucleic acid biologics, and immunotherapeutics [144,145,146,147,148,149,150,151,152]. AI algorithms can design proteins and peptides with desired features [153,154,155,156,157]. AI models can generate therapeutic sequences with improved stability, binding affinity, or immunogenicity by analyzing protein structure and function data, enabling customized biologics with enhanced effectiveness and safety [158,159]. Just as cybersecurity tools help design secure systems, AI tools help design biologics with desired therapeutic properties.
AI systems identify therapeutic targets using genetic, proteomic, and clinical data, aiding researchers in creating protein and peptide biologics that modulate biological pathways or target disease-causing proteins. AI models predict protein folding from amino acid sequences, crucial for understanding protein function and designing optimized biologics. Deep learning and molecular dynamics simulations can predict protein folding patterns, assisting in designing stable and functional biologics (Figure 6) [160].
Figure 6.
AI’s contribution to protein development and customized biologics includes data analysis, predictive modeling, and pattern recognition tools for improved protein development and customized proteins. Knowledge of altered biological pathways and disease target identification is required. AI facilitates protein folding prediction from amino acid sequences and deep learning and molecular dynamic simulation for better understanding, as well as protein/peptide binding affinity and toxicity prediction using SAR and toxicological datasets.
AI algorithms predict protein/peptide-target molecule binding affinity by training on protein-protein or protein-peptide datasets, reliably estimating binding strength, improving treatment effectiveness by selecting or creating biologics with high target affinity and specificity. AI optimizes protein and peptide biologic formulations, as biologic quality and effectiveness are affected by stability, aggregation tendency, and formulation factors. AI algorithms can optimize formulation conditions and biologic stability and shelf life by analyzing protein physicochemical parameters, formulation components, and manufacturing processes [161].
AI algorithms predict protein and peptide biologic toxicity by analyzing structure-activity relationships trained on toxicological datasets, anticipating biologic adverse effects and immunogenicity, allowing researchers to identify and alter harmful sequences or structures. AI optimizes clinical trials for protein and peptide biologics, predicting patient responses and refining trial procedures using patient data, illness features, and treatment results, streamlining patient enrollment, study design, and personalized treatment [162,163,164]. AI has the potential to significantly enhance research, diagnostics, and therapeutics in exosomes, CAR T-cell therapy, and CRISPR/Cas9 [164,165,166].
AI’s data analysis, pattern recognition, and predictive modeling capabilities accelerate protein/peptide and gene therapy biologic development, making therapeutic molecule design and optimization more efficient and targeted. AI revolutionizes the field by enabling novel biologics with enhanced properties and improving biologic development success rates [167].
5.5. AI in Medical Devices
Medical devices, including apparatus, implements, instruments, implants, machines, and reagents for specific medical purposes, can be used alone or with software or related systems in vitro to address patient medical issues. AI has significantly advanced medical devices, revolutionizing healthcare. Personalized medicine and remote health monitoring, accelerated by the pandemic, have boosted AI and machine learning applications in healthcare. Examples of AI utilization in medical devices include:
These examples illustrate AI integration into medical devices to enhance diagnostics, monitoring, treatment, and patient care. AI’s ability to analyze large data volumes, identify patterns, and provide personalized insights contributes to more accurate diagnoses, improved treatment outcomes, and better overall healthcare delivery, developing new products for patient benefits, reaching new customer segments, and creating more business potential. Medical technology companies are using AI in major sectors like diagnosis, prevention, care, and personalized medicine. The threat identification capabilities of AI can be applied to medical device cybersecurity, ensuring device safety and patient data protection.
For instance, Medtronic uses AI to help diabetes patients manage their condition. The Medtronic Guardian Connect system combines AI and continuous glucose monitoring (CGM) for real-time insights and support. Medtronic collaborated with IBM Watson in 2016 to develop the Medtronic Sugar IQ app, a mobile personal assistant for diabetes management, incorporating AI for features like “insights” (analyzing glucose patterns, identifying trends, providing personalized messages), “glycemic assistance” (real-time guidance based on glucose readings), and “food logging” (analyzing food impact on glucose levels). The Sugar IQ app helps users understand glucose patterns, provides real-time management assistance, and aids dietary decisions, improving disease management and patient control of diabetes [174,175,176,177,178].
6. AI for Pharmacokinetics and Pharmacodynamics
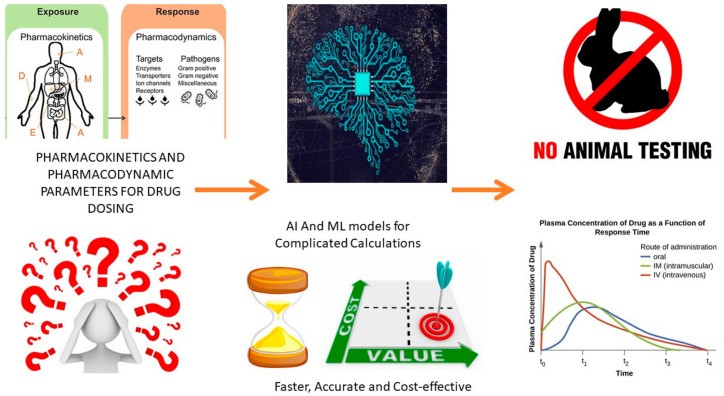
Drug development is complex, involving drug discovery, preclinical studies, clinical trials, and regulatory approval. Pharmacokinetics and pharmacodynamics are crucial, determining optimal dosage, administration route, and drug safety [85]. Traditional pharmacokinetic and pharmacodynamic study methods can be time-consuming, expensive, and may not accurately predict drug efficacy and safety [179,180].
Traditional pharmacokinetics and pharmacodynamics studies use animal studies and human clinical trials, facing ethical concerns, sample size limitations, and interindividual variability. These methods may not always accurately predict human drug pharmacokinetics and pharmacodynamics. Computational models and AI methods have been developed for faster, cost-effective, and more accurate drug pharmacokinetics and pharmacodynamics prediction [181,182].
AI shows significant potential in pharmacokinetics, pharmacodynamics, and drug discovery [183]. With powerful computing and machine learning algorithms, AI is valuable for predicting and optimizing drug pharmacokinetics and pharmacodynamics. Despite challenges of large and reliable datasets, AI opens new avenues in PKPD studies and therapy impacts [183,184,185,186,187]. Just as cybersecurity threat analysis is essential for understanding and mitigating digital risks, AI-driven PKPD analysis is essential for understanding and optimizing drug behavior in the body.
6.1. AI-Based Methods to Predict Pharmacokinetic Parameters
Machine learning (ML) and deep learning (DL) algorithms are prevalent in pharmacokinetic parameter prediction. ML algorithms like Bayesian models, random forests, support vector machines, ANNs, and decision trees predict drug absorption, distribution, metabolism, and excretion (ADME). DL algorithms, including CNNs, LSTMs, and RNNs, are used to predict pharmacokinetic parameters such as drug absorption, bioavailability, clearance, volume of distribution, and half-life. Quantitative structure–activity relationship (QSAR), a computational approach using chemical structure to predict biological activity, is applied in pharmacokinetics to anticipate drug ADME properties like solubility, permeability, and metabolism (Figure 7) [121,188,189,190,191].
Figure 7.
AI’s role in PKPD studies includes pharmacokinetic studies (absorption, distribution, metabolism, excretion) and pharmacodynamic studies (drug effects on targets). AI accelerates complex calculations, avoids missed datasets, and provides accurate, fast, cost-effective results, converting complex data into understandable graphs for root cause analysis. AI also minimizes animal studies by calculating impacts of conditions like enzymes, diseases, dosing, and patient data in different animals, reducing animal use in clinical trials.
6.2. AI-Based Computational Method for PBPK
PBPK models simulate drug distribution and clearance, but their development requires extensive data and computational resources. AI-based methods simplify PBPK model development by using machine learning algorithms to identify relevant model features (Table 4). AI-based computational methods also optimize PBPK model parameters, reducing the need for animal studies and human clinical trials [192,193,194]. Just as cybersecurity risk modeling helps predict and prepare for potential cyberattacks, AI-based PBPK modeling helps predict drug behavior in the body.
Drug efficacy and safety depend on pharmacokinetic parameters. Drug safety is based on active drug duration in the body, and dosage depends on elimination. In vivo exposure is crucial for drug safety and efficacy assessment. Drug discovery and development involve pre-clinical and clinical trial assessments. Absorption, distribution, metabolism, and elimination (ADME) are major factors in drug molecule attrition. Drug discovery studies use in vivo pharmacokinetic studies in animals, and in vitro systems are used for humans and animals. First-in-human dosing optimizes drug exposure in humans. In vitro and in vivo extrapolations are used for liver microsomes and hepatocytes. Hepatic clearance is assessed in vivo in humans and animals and in vitro using liver microsome studies. Human pharmacokinetic parameters are estimated using allometric scaling methods and in vivo preclinical data, estimating volume of distribution, drug clearance, and bioavailability. Mathematical frameworks and PBPK modeling simulate time course and ADME properties, understanding in vivo behavior for human extrapolation, typically applied in later drug discovery stages. In vivo data complexity exceeds in vitro pharmacokinetic parameters, and AI and ML are used for analysis and assessment [195].
6.3. Prediction of Drug Release and Absorption Parameters
AI-based models effectively predict drug release and absorption parameters. AI algorithms analyze data from drug delivery systems and predict drug release kinetics. Considering drug physicochemical properties, formulation characteristics, and delivery system release mechanisms, AI models estimate drug release rate and extent over time, predicting release kinetics from oral tablets, transdermal patches, and inhalers [196]. The predictive power of AI for drug release and absorption is analogous to the predictive capabilities of cybersecurity threat intelligence platforms.
AI-based models predict drug absorption parameters like bioavailability and absorption rate by considering drug solubility, permeability, and formulation characteristics. Analyzing drug physicochemical properties like lipophilicity and molecular weight, AI models correlate them with absorption data to estimate drug absorption efficiency into the bloodstream. AI-based models provide a powerful tool for predicting drug release and absorption parameters, optimizing drug formulations, guiding drug development decisions, and designing more effective drug delivery systems [189,190,191,192,193,194,197].
6.4. Prediction of Metabolism and Excretion Parameters
AI-based models are valuable in predicting drug metabolism and excretion parameters, providing insights into drug pharmacokinetics. AI algorithms analyze drug molecular structure and physicochemical properties to predict metabolic pathways, identifying structural features associated with specific metabolic transformations by training on drug metabolism datasets. These models predict potential metabolites and major enzymes involved in drug metabolism [198]. Just as cybersecurity incident response teams analyze attack patterns to understand and mitigate threats, AI analyzes drug metabolism patterns to understand and optimize drug behavior in the body.
AI-based models calculate enzyme kinetics to estimate drug metabolic fate, considering factors like enzyme expression levels, genetic variations, and drug-drug interactions to assess metabolism impact on drug clearance and efficacy, valuable for optimizing drug dosing regimens and predicting drug interactions [199].
AI algorithms predict drug clearance rates by analyzing drug physicochemical properties like molecular weight, lipophilicity, and ionization, training on datasets with drug clearance pathway information to estimate drug elimination rate, crucial for determining appropriate dosing regimens and ensuring drug efficacy and safety [200].
AI models predict drug interactions with transporters involved in ADME processes, considering drug physicochemical properties and transporter characteristics to assess potential drug-drug interactions or altered pharmacokinetics due to transporter effects, aiding drug disposition understanding and formulation optimization [201,202,203,204].
AI algorithms analyze vast drug metabolism and excretion data to predict drug fate, aiding drug dosing optimization, drug interaction identification, and safer, more effective medication design. AI models help prioritize drug candidates based on predicted metabolic and excretion profiles, facilitating efficient drug development processes.
Table 4.
Algorithms used for the development of AI models for various PKPD studies along with their advantages and limitations.
| Algorithm/Software | Aim/Target | Advantage | Limitation | PK/PD/Both | Reference |
|---|---|---|---|---|---|
| Bayesian/WinBUGS | To handle data below the limit of quantification | – Prior information from the literature can be directly used for model-fitting – Easy implementation | – Long computational time – Negative data in certain PK/PD models which are not possible | Both | [205] |
| Bayesian/PKBUGS (v 1.1)/WinBUGS (v 1.3) | Pharmacokinetic analysis of sirolimus concentration data for therapeutic drug monitoring | – Easy incorporation of prior information with current data – Identification of possible covariate relationship | – A limited number of datasets and poorly informative data | PK | [206] |
| Support Vector Machine/Least Square-SVM | Drug concentration analysis of sample drug based on individual patient profile | – Personalized model for every new patient – SVM-based approaches are more accurate than the PK modeling method for predicting drug concentration | – Outliers in samples greatly affect the model, limiting its accuracy | PK | [207] |
| Support Vector Machine/Drug Administration Decision Support System (DADSS) and Random Sample Consensus RANSAC | Prediction of drug concentration, ideal dose, and dose intervals for a new patient | – More flexible and structurally adjustable | – The noise of datasets impacts the overall predictability of the algorithm | PK | [208] |
| Support Vector Machine/Profile Dependent SVM | Therapeutic drug monitoring of kidney transplant recipient | – Critical dosing and cost-effective – Effective for nonlinear models | – Time-consuming – Large datasets | PK | [209] |
| Support Vector System + Random Forrest Model | Pharmacodynamic drug interaction based on Side-Effect Similarity (SES), Chemical Similarity (CS), and Target Protein Connectedness (TPC) | – PDI was predicted with an accuracy of 89.93% and an AUC value of 79.96% | – Requires larger data processing and filtration | PD | [210] |
| Linear Regressions (LASSO)/Gradient Boosting Machines/XGBoost/Random Forest | Prediction of the plasma concentration–time series and area under the concentration-versus-time curve from 0 to 24 h after repeated dosing of Rifampicin | – Time-efficient analysis – Improves method for covariate selections | – Risk of results being not clinically relevant | PK | [182] |
| XGBoost | Estimation of drug area under the curve (AUC) of tacrolimus or mycophenolate mofetil (MMF) | – Pharmacokinetic (PK) datasets from renal, liver, and heart transplant patients were predicted accurately | – Not possible to calculate the probability of target attainment and accurate dosing | PK | [211,212] |
| Simulated Annealing k-Nearest-Neighbor (SA-kNN)/Partial Least-Square (PLS)/Multiple Linear Regression (MLR)/Sybyl version 6.7 | Prediction of pharmacokinetic parameters of antimicrobial agents in humans based on their molecular structure | – Cost-effective – Requires less sample size | – Requires multiple model generation methods – Interpretation of individual descriptors is almost impossible | Both | [213] |
| Drug Target Interaction Convolutional Neural Network (DTICNN) | Identification of the drug-target interactions and predict potential drug molecules | – Cost-effective – Time-saving | – Large datasets are required | PD | [214] |
| Deep Long Short-Term Memory (DeepLSTM) | Computational methods to validate the interaction between drugs and target | – Based on Position Specific Scoring Matrix (PSSM) and Legendre Moment (LM) (drug molecular substructure fingerprints) | – Large datasets are required | PD | [215] |
7. Limitations of AI Tools
Despite their benefits, AI-based models have limitations like the need for large datasets, potential biases, and lack of interpretability. AI-based models should be used with traditional experimental methods to ensure drug safety and efficacy. Some limitations include:
7.1. Lack of Transparency
AI models, using complex algorithms, are often “black boxes,” making it hard to understand prediction processes. This lack of transparency can hinder regulatory approval and trust in AI-based drug development tools, especially if predictions conflict with clinician or researcher expectations [216,217]. Similarly, while cybersecurity threat identification tools are powerful, their inner workings can also be opaque, requiring trust in their effectiveness despite limited transparency.
7.2. Limited Availability of Data
AI models require large datasets for accurate predictions. Limited data for specific drugs or populations can lead to less accurate or biased results. Rare diseases may have limited data, challenging AI model development. Data used to train AI models may not represent the target population, causing bias. Unavailable data types, like longitudinal data or real-world evidence, can limit AI utility. Data quality and representativeness are crucial considerations.
7.3. Biases in Data
AI model efficacy and precision depend on training data quality. Biased or incomplete data can lead to biased predictions. Homogeneous patient populations in clinical trials are a problem. Underrepresentation of demographics or disease states in training datasets compromises model accuracy for those populations. Incomplete or inaccurate data can lead to erroneous assumptions and imprecise predictions. AI-guided clinical decision-making poses challenges. Training data must represent the target population and be trustworthy, comprehensive, and impartial [218,219]. Just as cybersecurity tools can be biased by the data they are trained on, AI in pharmaceuticals can be biased by patient data, leading to inaccurate or unfair outcomes.
7.4. Inability to Incorporate New Data
Updating trained AI models with new data can be challenging and resource-intensive, limiting adaptability to new drug introductions or clinical trial data. AI models must evolve with drug development changes. Failure to update can cause inaccurate predictions and flawed decisions. Strategies for easy model updates and continuous refinement are needed.
7.5. Limited Ability to Account for Variability
AI models trained on large datasets may be biased towards average responses, failing to accurately predict drug responses for individuals deviating from the average, especially concerning for drugs with wide response ranges in different patients, like in cancer [220].
7.6. Interpretation of Results
Complex AI models can generate outputs difficult to interpret, even for experts, lacking clear explanations for predictions, challenging clinician and researcher understanding and interpretation. Results may be hard to translate into actionable insights for clinical practice or drug development. AI model use may require technical expertise not readily available, limiting usefulness. Improved AI model interpretability and explainability are needed for effective use [221,222]. The interpretability of AI results is crucial, just as understanding the output of cybersecurity threat analysis tools is necessary for effective security responses.
7.7. Ethical Considerations
AI use in drug development raises ethical concerns, including patient privacy with sensitive health data used for AI model training. Data safety and security are crucial. Patient data collection and use must protect privacy and respect rights. Data ownership is another concern, with data collected without explicit consent, causing conflicts between patients, researchers, and pharmaceutical companies [223,224]. Regulatory agencies must develop stringent protocols, guidelines, and evaluation processes for AI integration in drug development, addressing ethical considerations, animal welfare, and patient safety. Animal testing requires reducing, refining, and replacing animal models. AI models must undergo thorough validation for reliability and accuracy to prioritize patient safety. The FDA discussion paper on AI and machine learning in drug and biological product development is an important step, outlining AI’s role and recommended practices, marking a milestone in regulating AI in healthcare and paving the way for regulatory advancements [225]. Ethical considerations and regulatory frameworks are as crucial for AI in pharmaceuticals as they are for cybersecurity, where responsible and ethical use of powerful technologies is paramount.
7.8. Complex Biological Systems
AI’s ability to fully mimic biological system complexity is limited. Biological systems are intricate, dynamic, with interconnected pathways, feedback loops, and molecular interactions. This complexity challenges AI models, which often simplify biological processes. AI models rely on training data, which may not fully capture biological system intricacies [226]. Genetic variations, environmental conditions, and interindividual variability contribute to complexity and variability not fully captured by AI models [45,227]. Emergent properties of biological systems, system-level behaviors from collective component behavior, are hard to predict solely from individual component properties. Limited understanding of biological processes hinders accurate AI model incorporation [228].
7.9. Lack of Clinical Expertise
AI identifies correlations, but individual patient therapies can vary despite these correlations. AI algorithms operate statistically, limiting their understanding of intricate factors and parameter effects. Complex treatment decisions influenced by individualized factors pose challenges for statistical AI models [229]. AI’s ability to fully capture critical aspects and implications of specific parameters may be limited, necessitating clinical expertise in interpreting AI-driven insights.
7.10. Inactive Molecules
AI predicts small molecule-target protein binding interactions computationally, but simulations can identify inactive molecules. Accurately representing conformational flexibility of small molecules and target proteins is challenging, as docking algorithms sample limited conformations, causing false positives or negatives in binding affinities [34]. Incomplete or inaccurate protein structures used in docking or AI can lead to erroneous predictions. Difficulties accounting for solvation effects, receptor flexibility, and other factors limit docking. Experimental validation is crucial to confirm compound activity, potency, and selectivity. Refining docking algorithms, scoring functions, and incorporating protein flexibility and solvent effects aim to improve docking-based screening reliability. Integrating computational methods like molecular dynamics simulations can provide a more comprehensive representation of molecular interactions [230]. Similarly, cybersecurity threat identification tools can sometimes produce false positives, requiring expert validation to distinguish real threats from harmless anomalies.
Despite AI tool limitations, their potential in pharmaceutical development is significant. Addressing these limitations is crucial for industry advancement. Recent progress in data availability, deep learning algorithms, explainability, integration with other modeling approaches, and computational power helps resolve challenges [231].
Misreported data, causing bias and distorting AI model accuracy, remains a persistent problem. Adopting FAIR data principles (Findable, Accessible, Interoperable, Reusable), aligning with ALCOA (Attributable, Legible, Contemporaneous, Original, Accurate) principles, is imperative to improve data quality and enhance AI-driven analysis reliability [232].
AI in PKPD studies faces substantial challenges that require time to overcome, but continuous field evolution offers hope for improvement. Caution is needed, avoiding over-reliance on AI without considering limitations and verifying results through rigorous scientific validation. AI, while potent, assists researchers and clinicians in data analysis, pattern identification, and prediction, but it is not ready to replace human expertise in PKPD studies. Successful PKPD studies require collaboration between AI and human experts. AI integration in pharmaceutical research should be balanced, acknowledging both potential and the need for careful evaluation and validation.
8. Current Trend: Fairy Tale to the Holy Grail
Current trends show AI’s wide impact in pharmaceutics across drug discovery, precision medicine, formulation optimization, clinical trials, safety monitoring, and supply chain management. Prominent trends include:
- Drug Discovery and Development: AI revolutionizes drug discovery via virtual screening, molecular modeling, and predictive analytics, analyzing vast chemical and biological data to identify drug candidates, optimize lead compounds, and predict properties, accelerating novel therapeutic identification and development.
- Precision Medicine: AI advances precision medicine by analyzing patient data (genomics, proteomics, clinical records) to identify subgroups, predict treatment responses, and aid personalized treatment decisions, also contributing to biomarker development for diagnosis and prognosis.
- Drug Repurposing: AI identifies new uses for existing drugs by analyzing large datasets and biological knowledge, identifying drug-disease associations and repurposing approved drugs for new indications, offering faster, cost-effective drug development.
- Drug Formulation and Delivery: AI optimizes drug formulations and delivery systems, predicting drug release kinetics and absorption profiles, and optimizing formulations for enhanced efficacy and targeted delivery, also designing drug delivery devices and systems for improved patient adherence and convenience.
- Clinical Trial Optimization: AI optimizes clinical trials, improving efficiency and reducing costs, aiding patient recruitment, identifying trial populations, optimizing protocols, and assisting in real-time trial data monitoring and analysis for adaptive designs and faster decision-making.
- Regulatory Compliance and Safety: AI increasingly supports regulatory compliance and drug safety, analyzing real-world data, adverse event reports, and literature to identify safety issues and monitor post-marketing drug safety, also aiding pharmacovigilance, signal detection, and adverse event prediction.
- Supply Chain Optimization: AI optimizes pharmaceutical supply chains, ensuring efficient manufacturing, inventory management, and distribution, predicting demand, optimizing production schedules, and enhancing quality control, contributing to streamlined, cost-effective operations. Just as cybersecurity threat intelligence helps optimize security operations, AI helps optimize pharmaceutical supply chains.
Pharmaceutical companies increasingly recognize AI’s potential in PKPD studies, leveraging AI to analyze large datasets, predict drug-target interactions, optimize drug candidates, and simulate drug responses. Examples include GNS Healthcare [233], AstraZeneca [234], Atomwise [235], Recursion Pharmaceuticals, and Insilico Medicines [236]. AI has improved strategies for rapid, accurate dosage form development. Pfizer uses AI to predict drug-drug interactions (DDIs) by analyzing drug structures, clinical outcomes, and adverse effects [237], efficiently identifying potential DDIs and prioritizing drug combinations for investigation, minimizing adverse reaction risks. Novartis leverages AI in drug formulation and delivery optimization, using algorithms to analyze physicochemical properties, solubility, and permeability data for optimal formulations and delivery systems, streamlining drug development and improving bioavailability and therapeutic efficacy. Roche integrates patient-specific data into AI models for personalized medicine [238], predicting individual drug responses and tailoring treatment regimens using genetic profiles, medical histories, and biomarkers for more effective, personalized therapies. These examples highlight AI’s innovative use by pharmaceutical companies in PKPD studies, paving the way for enhanced drug development and improved patient outcomes. Table 5 lists major AI applications in pharmaceutical companies.
Table 5.
Lit of companies using AI and ML technologies in pharmaceutical research [239].
| Sr. No. | Domain | Technology and Outcome | Industry and Collaborations |
|---|---|---|---|
| 1 | Drug design | Novel therapeutic antibodies | Exscientia |
| 2 | Molecular drug discovery | AtomNet–deep learning-driven computational platform for structure-based drug design | AtomWise |
| 3 | Gene mutation related disease | Machine learning based recursion operating system for biological and chemical datasets | Recursion |
| 4 | Drug design | Ligand- and structure-based de novo drug design, especially in multiparametric optimization | Iktos |
| 5 | Drug discovery | Generative modeling AI technology | Iktos and Galapagos |
| 6 | Drug development | Potential preclinical candidates | Iktos and Ono Pharma |
| 7 | Drug design | Rapid drug design by software “Makya” | Iktos and Sygnature Discovery |
| 8 | Drug discovery and Drug development | Pharma.AI, PandaMics, ALS.AI | Insilico Medicine |
| 9 | Drug target and Drug development | ChatPandaGPT | Insilico Medicine |
| 10 | Drug development | Protein motion in drug development lie RLY-4008 (Novel allosteric, pan mutant and isoform selective inhibitor of PI3Kα | Relay therapeutics |
| 11 | Drug discovery | AI and machine learning for selection of drug target | BenevolentAI |
| 12 | Drug target | Drug target selection for chronic kidney disease and idiopathic pulmonary fibrosis | BenevolentAI and AstraZeneca, GlaxoSmithKline, Pfizer |
| 13 | Clinical trials | AI in clinical trials | Pfizer and Vysioneer |
| 14 | Disease treatment | AI and supercomputing for oral COVID-19 treatment Paxloid | Pfizer |
| 15 | Drug discovery | NASH drugs and sequencing behemoth Illumina | AstraZeneca and Viking therapeutics |
| 16 | Drug development | Trials360.ai platform in clinical trials for site feasibility, site engagement and patient recruitment | Janssen |
| 17 | Drug research | Automate medical literature review by using natural language processing | Sanofi |
| 18 | Drug development | AI in drug development | BioMed X and Sanofi |
| 19 | Drug research and drug development | AI empowerment and AI exploration platforms | Novartis and Microsoft |
| 20 | Drug discovery | AI drug discovery platform | Bayer |
9. Futuristic Overview
AI may revolutionize the pharmaceutical industry, accelerating drug discovery and development. Virtual screening will rapidly analyze chemical libraries, finding therapeutic candidates with required features, speeding lead compound identification. AI-enabled precision medicine could categorize patients, predict therapy responses, and customize medicines by analyzing genomes, proteomes, and clinical records. Scientists may create innovative compounds with target-binding characteristics using deep learning and generative models, improving medication effectiveness and reducing adverse effects. AI will enable patient-specific dose formulations, optimizing compositions and delivery methods for improved treatment results by considering patient-specific parameters. AI algorithms will revolutionize safety assessment by predicting drug candidate side effects and toxicity. Future cybersecurity threat identification tools will likely incorporate AI for even more proactive and sophisticated threat detection.
AI-powered monitoring systems will enable remote patient care and medication adherence. Wearable devices and sensors will continuously gather data for AI algorithms to propose personalized therapy and better compliance. AI improves clinical trial design, patient selection, and recruitment, using electronic health records, biomarkers, and genetic profiles to find suitable patients, lower trial costs, and speed up approval.
AI models will optimize continuous manufacturing operations through real-time monitoring and control of key parameters, making pharmaceutical manufacturing uniform and efficient via data analysis and feedback. AI will analyze large amounts of data to inform regulatory decisions, assisting regulatory bodies in speeding up medication approval and improving safety.
AI use in healthcare segments is growing daily, from triage and screening to clinical risk prediction and diagnosis [141,240]. Clinical AI applications can increase diagnosis accuracy and healthcare efficiency. The vast time and money spent on medication R&D necessitate more inventive methodologies [241]. AI provides opportunities in medicine like multivariate data analysis, resolving complex drug delivery system creation issues, improving decision accuracy, disease categorization, modeling, formulation-processing factor correlation, dosage ratio optimization, rapid drug development, drug bioactivity and interaction prediction, cellular response, combination drug effectiveness, treatment outcomes, and more. AI and machine learning have potential to revolutionize medication delivery for improved infectious disease treatment. However, practical AI uses in medication delivery, especially therapeutically, are currently limited. Various AI methods in drug delivery for infectious diseases, such as Boost, 𝑘-nearest neighbors, decision trees, random forests, Naïve Bayes, ANN, Feedback System Control (FSC), SVM, Set Covering Machine (SCM), and logistic regression, have not been widely evaluated or used clinically, indicating clinical translation hurdles [96,144]. Machine learning and AI with PBPK modeling are important for drug development and environmental chemical risk assessment. Recently developed PBPK models describe chemical entry, bioavailability, tissue drug movement, and drug metabolism and elimination mathematically. PBPK-based toxicity models are suitable for nanomaterial toxicity determination. Developing mechanistically valid PBPK models for novel compounds with limited prior knowledge is complex due to poorly described chemical ADME routes. Neural-ODE (Neural-ordinary differential equation) algorithms now enable PBPK simulations for novel medications based on properties, learning governing ODE equations algorithmically from PK data without prior knowledge. AI approach advancements, especially deep neural network models, may help solve current challenges, improving PK and PBPK modeling and simulation performance for drug discovery, development, and human health risk assessment of environmental chemicals [242]. AI in PKPD development ultimately depends on understanding scientific principles, requiring standard regulations with strict measures to prevent AI abuse while accelerating growth, necessitating collaboration among pharmaceutical companies, regulatory bodies, healthcare professionals, and data scientists.
While this futuristic overview offers exciting possibilities, data quality, regulatory frameworks, and ethical guidelines must be addressed for full AI potential realization in pharmaceutical product development. Continued advancements and collaborations between industry, academia, and regulatory bodies indicate AI-driven innovations can revolutionize the pharmaceutical industry and improve patient outcomes in the future.
10. Conclusions
AI is transforming drug delivery technologies, enabling targeted, personalized, and adaptive therapies, enhancing drug efficacy, minimizing side effects, and improving patient outcomes through data analysis, pattern recognition, and optimization. AI-based methods have revolutionized pharmacokinetics and pharmacodynamics, offering advantages over traditional methods, predicting pharmacokinetic parameters, simulating drug distribution and clearance, and optimizing dosage and administration routes. AI-based computational methods for PBPK models simplify model development and parameter optimization, reducing animal and human clinical trial needs. Computational pharmaceutics, facilitated by AI and big data, revolutionizes drug delivery, providing efficient, cost-effective, data-driven approaches, optimizing formulations, personalizing therapies, ensuring regulatory compliance, and reducing risks, improving drug manufacturing and patient outcomes. AI technology integration holds great promise for accelerating drug development, improving patient outcomes, and revolutionizing the pharmaceutical industry, driving its evolution from era 4.0 to 5.0. Just as cybersecurity is evolving to meet new digital threats, AI in pharmaceuticals is evolving to address new challenges and opportunities in drug development and patient care.
Author Contributions
Conceptualization L.K.V.; validation, L.K.V. and V.P.C.; formal analysis, L.K.V. and V.P.C.; resources, R.R.S.T. and L.K.V.; writing—original draft preparation, A.D.G., K.J., V.P.C. and H.K.S.; review and editing, L.K.V. and V.P.C.; supervision, L.K.V. and R.R.S.T. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not Applicable.
Informed Consent Statement
Not Applicable.
Data Availability Statement
No new data were created or analyzed in this study. Data sharing is not applicable to this article.
Conflicts of Interest
The authors declare no conflict of interest in this study.
Funding Statement
This research received no external funding.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No new data were created or analyzed in this study. Data sharing is not applicable to this article.

