Introduction
Effective pain management in children, especially those with intellectual and developmental disabilities (IDDs), presents a significant challenge in healthcare. Children with conditions like cerebral palsy (CP) frequently undergo major orthopedic surgeries, and their ability to articulate their pain can be compromised due to communication barriers. This can lead to underestimation and inadequate treatment of postoperative pain, impacting recovery and quality of life. While pain assessment tools have improved, a universal solution for nonverbal children remains elusive. Proxy measures and trial-and-error approaches are often relied upon, highlighting the need for objective and reliable pain assessment methods.
Among the promising tools available is the Critical-Care Pain Observation Tool (CPOT). Initially designed for critically ill adults unable to self-report pain, CPOT has demonstrated validity across diverse adult populations, including postoperative and intensive care settings. Experts recommend CPOT due to its robust psychometric properties and validation in multiple languages. Its key advantages include a brief 1-minute observation period, objectivity by excluding family input, and straightforward scoring, potentially reducing training demands. However, its application in pediatric contexts requires further exploration. This article delves into the Critical-Care Pain Observation Tool, its validation in pediatric settings, and how video resources can enhance understanding and implementation for healthcare professionals.
The Need for Objective Pain Assessment in Pediatric Postoperative Care
Postoperative pain is a significant concern for all patients, but it poses unique challenges in pediatric populations, particularly those with IDDs. Conditions like cerebral palsy often necessitate major orthopedic interventions to address musculoskeletal complications such as hip dislocation and spinal deformities. These surgeries, while crucial for improving mobility and function, are inherently painful and require diligent postoperative pain management.
Children and adolescents with CP are known to experience more complex and prolonged hospitalizations compared to their neurotypical peers undergoing similar orthopedic procedures. Spinal fusion surgery, a common procedure for both CP patients and those with adolescent idiopathic scoliosis, is particularly invasive and associated with persistent postoperative pain. Effective pain resolution and management are paramount to the success of such interventions, as unrelieved pain can lead to emotional distress, prolonged opioid use, and delayed recovery.
Research indicates a potential disparity in postoperative pain management for children with IDDs. Studies have shown that patients able to self-report pain often receive more aggressive pain management, such as higher doses of opioids, compared to those with communication barriers. This suggests a risk of undertreatment in nonverbal pediatric patients, underscoring the urgent need for reliable and objective pain assessment tools like the Critical-Care Pain Observation Tool (CPOT).
Limitations of Existing Pediatric Pain Assessment Tools
While significant progress has been made in developing pain assessment tools for children with IDDs, several challenges remain. The heterogeneity in cognitive function and verbal abilities within this population makes a one-size-fits-all approach ineffective. Many existing tools, while validated, may have limitations in clinical utility.
Tools like the Non-Communicating Children’s Pain Checklist–Postoperative Version (NCCPC-PV) and the Pediatric Pain Profile (PPP), while reliable, can be complex and time-consuming to administer. Their broader scoring ranges may also hinder intuitive pain intensity interpretation. The PPP, for instance, requires extensive preparation, including parental interviews to personalize assessment criteria, which may be impractical in acute postoperative settings.
Conversely, tools like the revised Face, Legs, Activity, Consolability, Cry Scale (rFLACC) and the Individualized Numeric Rating Scale (INRS) offer quicker administration. However, the INRS, while rapid, demands initial individualization, potentially delaying implementation. Furthermore, individualized tools relying on parental input can be susceptible to bias. Parental interpretations of a child’s pain behaviors may not always be accurate, especially in situations involving Munchausen by proxy or parental impairment.
These limitations highlight the need for a pain assessment tool that is objective, efficient, and easily interpretable in the pediatric postoperative setting. The Critical-Care Pain Observation Tool (CPOT) emerges as a promising candidate due to its established validity in adult critical care and its potential for adaptation to pediatric populations.
Introducing the Critical-Care Pain Observation Tool (CPOT)
The Critical-Care Pain Observation Tool (CPOT) is a behavioral pain assessment scale initially developed to evaluate pain in critically ill adult patients who are unable to self-report. Its foundation lies in observing specific behavioral indicators of pain, eliminating reliance on subjective patient reporting, which is often challenging or impossible in critical care settings.
CPOT assesses four key behavioral categories:
- Facial Expressions: Observing for signs of relaxation, tension, or grimacing.
- Body Movements: Noting immobility, protective movements, or restlessness/agitation.
- Muscle Tension: Assessing muscle tone as relaxed, tense, or very tense (rigid).
- Vocalization (for non-intubated patients) or Ventilator Compliance (for intubated patients): Evaluating vocalizations like absence of sound, normal speech, sighing, moaning, crying out, or sobbing in non-intubated patients. For intubated patients, it assesses their compliance with the ventilator, such as tolerating movement, coughing, or fighting the ventilator.
Each behavior is scored on a scale of 0 to 2, resulting in a total CPOT score ranging from 0 to 8. A higher score indicates a greater likelihood of pain. It is crucial to note that CPOT is designed to detect the presence of pain based on the number and intensity of observed behaviors and does not directly quantify pain intensity on a numerical scale.
CPOT’s strengths lie in its objectivity, brevity, and ease of use. Its 1-minute observation period is clinically practical, and the exclusion of family input minimizes potential bias. The straightforward scoring system simplifies interpretation and potentially reduces the training burden for healthcare staff. These attributes make CPOT an attractive option for pain assessment in pediatric postoperative care, particularly for nonverbal or communication-challenged children.
Validation of CPOT in Pediatric Postoperative Patients: A Study on Spinal Fusion Surgery
Recognizing the potential of CPOT in pediatric pain management, a research study was conducted to validate its use in children and adolescents undergoing posterior spinal fusion surgery. This study aimed to assess CPOT’s effectiveness in detecting pain in this specific postoperative pediatric population, paving the way for its application in children with IDDs undergoing similar procedures.
The study employed a repeated-measure, within-subject design, involving 24 patients aged 10-18 years scheduled for posterior spinal fusion surgery for adolescent idiopathic scoliosis. Patients were able to self-report pain, allowing for comparison between CPOT scores and self-reported pain intensity.
The study focused on three key aspects of validation:
- Discriminative Validation: Assessing CPOT’s ability to differentiate between painful and non-painful stimuli. This was examined by comparing CPOT scores during a non-nociceptive procedure (gentle touch) and a nociceptive procedure (turning from back to side, a routine nursing procedure known to cause pain post-spinal fusion).
- Criterion Validation: Evaluating the correlation between CPOT scores and patients’ self-reported pain intensity using the Faces Pain Scale–Revised.
- Reliability: Assessing both interrater (agreement between different raters) and intrarater (consistency of a single rater over time) reliability of CPOT scores. Bedside raters and video raters were utilized to evaluate reliability under different observation conditions.
Patients were assessed on the day following surgery, with CPOT scores and self-reports collected before, during, and after both procedures. Behavioral reactions were video-recorded for retrospective analysis by independent video raters. All raters underwent standardized training on CPOT administration and scoring.
Key Findings: CPOT as a Valid Tool for Pediatric Postoperative Pain Assessment
The study yielded significant findings supporting the validity and reliability of CPOT for pediatric postoperative pain assessment:
-
Discriminative Validation: CPOT scores were significantly higher during the nociceptive turning procedure compared to the non-nociceptive touch procedure across all rater groups (bedside and video raters). This demonstrates CPOT’s ability to effectively discriminate between painful and non-painful stimuli in postoperative pediatric patients.
-
Criterion Validation: A moderate positive correlation was found between CPOT scores and patients’ self-reported pain intensity during the nociceptive procedure. This indicates that CPOT scores align reasonably well with patients’ subjective pain experiences, further supporting its validity as a pain assessment tool.
-
Reliability: While interrater reliability between bedside and video raters was found to be poor to moderate, intrarater reliability for video raters was moderate to excellent. This suggests that while real-time bedside assessments may have some variability, CPOT scoring is consistent when raters review video recordings, highlighting the potential for video-based training and assessment standardization.
-
Cutoff Score: A CPOT cutoff score of ≥2 was associated with optimal sensitivity (61.3%) and specificity (94.1%) for detecting pain. This cutoff score, consistent with findings in adult studies, provides a clinically useful threshold for identifying patients likely to be experiencing pain.
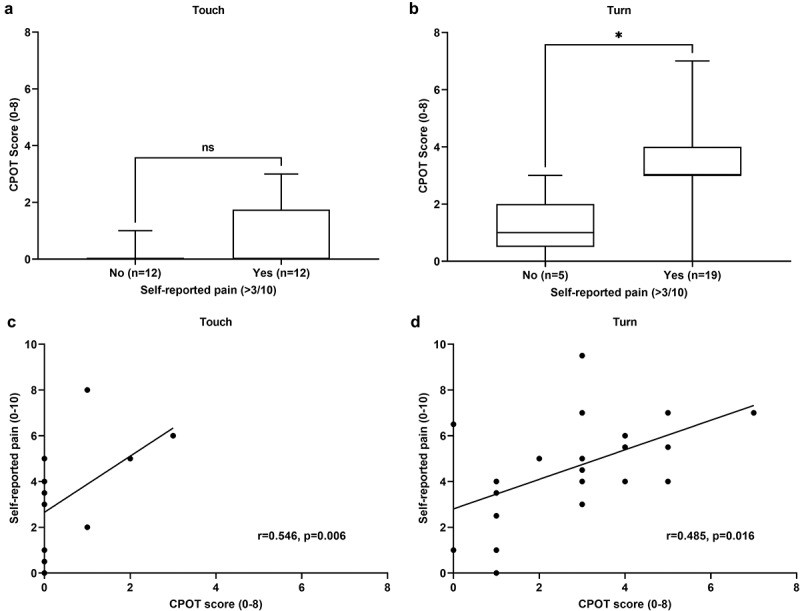 Figure 2.U test. The data are presented as the line within the box representing the median, upper and lower limits of the box representing the 25th and 75th percentiles, and the whiskers representing the range.
Figure 2.U test. The data are presented as the line within the box representing the median, upper and lower limits of the box representing the 25th and 75th percentiles, and the whiskers representing the range.
These results collectively suggest that the Critical-Care Pain Observation Tool (CPOT) holds promise as a valid tool for detecting pain in pediatric patients in the acute postoperative inpatient care unit following posterior spinal fusion surgery.
The Role of “Critical Care Pain Observation Tool Video” in Enhancing CPOT Implementation
The study’s findings underscore the potential of CPOT in pediatric postoperative pain management. However, effective implementation relies on proper training and standardization of assessment techniques. This is where “Critical Care Pain Observation Tool Video” resources become invaluable.
Video-based training offers several advantages:
- Standardization: Videos can demonstrate standardized CPOT administration and scoring techniques, reducing interrater variability and ensuring consistent application across healthcare providers.
- Visual Learning: CPOT involves observing subtle behavioral cues. Video demonstrations can effectively illustrate these cues, making it easier for clinicians to learn and recognize pain indicators in real-time.
- Accessibility and Scalability: Video resources are readily accessible and can be used for training large numbers of healthcare professionals efficiently, regardless of location.
- Self-Paced Learning: Clinicians can review training videos at their own pace, reinforcing their understanding and improving retention.
- Demonstration of Clinical Scenarios: Videos can depict diverse clinical scenarios, including patients exhibiting varying pain levels and responses to different procedures, enhancing clinicians’ preparedness for real-world application.
By incorporating “critical care pain observation tool video” into training programs, healthcare institutions can significantly enhance the adoption and consistent use of CPOT in pediatric postoperative care. These video resources can serve as a cornerstone for standardized training, ensuring clinicians are proficient in utilizing CPOT to objectively assess and manage pain in their young patients.
Implications and Future Directions
The validation of CPOT in pediatric postoperative patients undergoing spinal fusion surgery represents a significant step forward in improving pain management for this vulnerable population. The study’s findings suggest that CPOT can be a valuable tool for clinicians to objectively detect pain, particularly during painful procedures. The high specificity of CPOT may help prevent overtreatment with analgesics in patients who are not experiencing pain.
However, the study also highlights areas for further research and refinement:
- Generalizability: Further research is needed to validate CPOT in broader pediatric orthopedic surgery populations and across different age groups, including younger children and infants.
- Sensitivity to Analgesia: Future studies should investigate CPOT’s sensitivity to changes in pain levels following analgesic administration.
- Assessment of Evoked Pain: Research is needed to determine CPOT’s effectiveness in detecting pain evoked by active movement and other stimuli beyond passive turning.
- Application in Nonverbal Children: The ultimate goal is to validate CPOT for use in nonverbal pediatric patients, particularly those with IDDs. Future studies should focus on adapting and validating CPOT in this specific population.
- Interrater Reliability Improvement: Strategies to enhance interrater reliability in real-time bedside assessments need to be explored, potentially through more intensive training programs and ongoing competency assessments.
Figure 1. Discriminative validation of the Critical-Care Pain Observation Tool. The CPOT scores for each assessment are summarized for the (a) bedside rater, (b) video rater 1, and (c) video rater 2. The data are presented as the line within the box representing the median, upper and lower limits of the box representing the 25th and 75th percentiles, and the whiskers representing the range. Friedman rank sum tests revealed a significant difference in CPOT scores across the assessments for all raters. Post hoc Wilcoxon tests revealed only a significant difference in CPOT scores before and during the turning procedure and during and postprocedure but not between pre- and post-procedure.
Conclusion
The Critical-Care Pain Observation Tool (CPOT) demonstrates significant potential as an objective and reliable tool for assessing postoperative pain in pediatric patients, particularly those undergoing spinal fusion surgery. Its validity and reliability, as supported by research findings, position CPOT as a valuable asset in improving pain management in this vulnerable population. The integration of “critical care pain observation tool video” resources into training and implementation strategies can further enhance its effectiveness and ensure consistent, standardized pain assessment practices. As research continues to expand our understanding of CPOT’s application in diverse pediatric contexts, it holds promise for becoming a cornerstone of pediatric pain management, particularly for children who cannot effectively communicate their pain verbally.
