Depression stands as a widespread mental health disorder affecting millions of adults across the United States, necessitating effective strategies for early detection and intervention within primary care settings. Recognizing this critical need, the U.S. Preventive Services Task Force (USPSTF) advocates for routine depression screening in primary care, coupled with evidence-based treatment protocols. This article delves into the application of depression tools within primary care, drawing upon a quality improvement project that implemented VitalSign6, a measurement-based care (MBC) program, at an academic medical center. By examining the effectiveness of this program, we aim to highlight the significance of depression screening tools and measurement-based care in improving patient identification, treatment, and overall satisfaction in primary care environments.
Background: The Imperative for Depression Screening in Primary Care
Depression’s substantial prevalence in the U.S., affecting an estimated 17.3 million adults annually, underscores its significance as a public health concern. The disorder’s impact extends beyond emotional distress, contributing to significant disability, diminished productivity, and substantial economic burden, estimated at $210 billion each year. Untreated depression not only inflicts emotional suffering but also impairs relationships, reduces work performance, and elevates the risk of comorbid health conditions. The intricate link between mental and physical well-being further emphasizes the importance of addressing depression, especially in individuals with chronic diseases.
The robust evidence base supporting depression screening and treatment in primary care highlights its role in enabling timely identification and intervention. Recommendations from the USPSTF and endorsements from organizations like the American Academy of Family Physicians advocate for universal depression screening for adults in primary care. Furthermore, value-based payment models from the Centers for Medicare & Medicaid Services (CMS) reinforce these recommendations, incentivizing healthcare organizations to prioritize depression screening and follow-up care.
Landmark studies such as the Sequenced Treatment Alternatives to Relieve Depression (STAR*D) trial have demonstrated the feasibility and effectiveness of depression care within primary care settings. Despite compelling evidence and national guidelines, a significant gap persists, with over half of primary care patients with depression remaining undiagnosed and undertreated. National data reveals alarmingly low depression screening rates in primary care settings, highlighting the urgent need for improved implementation of screening protocols and effective depression tools.
Efforts to bridge this gap and enhance depression care in primary care increasingly focus on the adoption of validated screening tools. Among these, the Patient Health Questionnaire (PHQ)-2 and PHQ-9 stand out as the most widely utilized and clinically effective instruments for adult depression screening. The PHQ-2 serves as an initial screening step, efficiently identifying individuals who may require further evaluation with the more comprehensive PHQ-9. These tools offer primary care providers practical and reliable methods for identifying potential depression cases within their patient populations.
Research consistently underscores that optimal depression care outcomes and sustained remission are achieved through integrated systems of care that combine screening with structured treatment protocols and referral pathways. Measurement-based care (MBC) embodies this comprehensive approach, offering a framework that incorporates validated screening tools, standardized symptom assessments, treatment monitoring, and evidence-based decision support. MBC equips primary care physicians with the resources necessary for accurate diagnosis, tailored treatment planning, effective follow-up, and timely referrals, ultimately enhancing the quality of depression care delivered in primary care settings. The ongoing evolution of technology holds promise for further optimizing the integration of screening and MBC tools into primary care workflows, ensuring seamless and efficient implementation.
Purpose and Specific Aims of Implementing Depression Screening Tools
This quality improvement project was designed to implement VitalSign6, an evidence-based MBC program incorporating depression screening tools, within the Department of Family and Community Medicine at the University of Texas Southwestern Medical Center (UTSW). The overarching goal was to enhance the identification and management of depression among adult patients aged 18 and older. Specific aims included:
- Achieving a 75% screening rate for depression using the PHQ-2 among unique patients.
- Ensuring 85% of patients screening positive on the PHQ-2 undergo further screening with the PHQ-9.
- Administering MBC to 75% of patients diagnosed with depression and scheduling follow-up appointments within 4 to 6 weeks.
- Utilizing VitalSign6 MBC to monitor treatment responses, effects, and remission rates.
- Evaluating physician and staff satisfaction with the VitalSign6 program and its integration with the electronic health record (EHR).
These targets were informed by the VitalSign6 Primary Care First Model, establishing benchmarks for depression screening and MBC implementation in primary care.
Methods: Integrating Depression Tools into Primary Care Workflow
A pre-post intervention design was employed to assess the impact of implementing depression screening tools and MBC on screening rates, clinical outcomes, and satisfaction within the UTSW Department of Family and Community Medicine. The project received Institutional Review Board approval with a waiver for informed consent.
The clinic setting encompassed a residency program and a diverse patient population. The project timeline spanned from February to May 2019, with initial screening conducted throughout this period and follow-up care extending for 14 weeks for patients diagnosed with depression and receiving MBC.
Evidence-Based Innovation: VitalSign6 and Measurement-Based Care
The project leveraged VitalSign6, a web-based MBC program developed by the CDRCC, which provides primary care providers with essential tools for standardized depression care. VitalSign6 facilitates symptom severity assessment, monitoring of antidepressant side effects, adherence tracking, and algorithm-driven medication selection with decision support. By utilizing VitalSign6, primary care providers can personalize treatment strategies, ensuring evidence-based medication choices, appropriate dosages, timely referrals, and guideline-concordant follow-up care.
The VitalSign6 software streamlined the administration of depression questionnaires via iPads, available in both English and Spanish. Patients completed self-reported measures during check-in, integrating seamlessly with the clinic’s existing workflow. Providers could then access results in real-time, document diagnoses, and initiate tailored treatment plans with clinical decision support (CDS) features. For patients screening negative, VitalSign6 automatically scheduled rescreening for depression in one year.
Prior successful implementations of VitalSign6 in community-based clinics affiliated with UTSW paved the way for its integration into the Department of Family Medicine and Community Health. To address potential interoperability challenges with the EHR, a UTSW technology team developed an application programming interface utilizing Fast Healthcare Interoperability Resources (FHIR) and Substitutable Medical Apps Reusable Technology (SMART). This innovation enabled real-time integration of VitalSign6 directly within the Epic EHR system. Physicians could launch VitalSign6 contextually within Epic, review patient data, access CDS, and seamlessly document treatment plans within the patient’s EHR chart, as illustrated in Figure 1.
Figure 1. VitalSign6 Integration with Epic EHR System
Figure 1. VitalSign6 integration with Epic. This illustrates the seamless integration of VitalSign6 with the Epic Electronic Health Record (EHR) system, highlighting the accessibility of depression screening and management tools within the primary care provider’s workflow.
Clinic Training and Stakeholder Engagement
To ensure successful implementation, project leaders engaged with departmental leadership and clinical staff to optimize workflow integration and minimize disruptions. Comprehensive two-hour training sessions were conducted for physicians, residents, and clinic staff, covering depression education, screening protocols, symptom severity assessment, diagnostic procedures, evidence-based treatment practices, medication management, dosing guidelines, and referral processes. VitalSign6 expert trainers provided on-site support for two weeks post-implementation to address immediate needs and facilitate smooth adoption.
Procedure: Step-by-Step Depression Screening and Management
Initial Screening Protocol
Prior to screening, patients acknowledged an approved Patient Acknowledgement Form. Upon arrival for their initial visit, patients were provided with an Epic Welcome tablet to complete the PHQ-2 questionnaire. PHQ-2 scores were electronically transferred to the patient’s EHR. Patients scoring ≤2 on the PHQ-2 and lacking a documented history of depression or treatment proceeded with routine clinic workflow.
Patients screening positive on the PHQ-2, or those with a negative screen but a documented history of depression or antidepressant medication, triggered a Best Practice Advisor (BPA) alert. This BPA prompted nurses to administer the 9-item PHQ-9 using VitalSign6 on iPads to evaluate symptom severity. Patient-reported PHQ-9 scores were then directly integrated into the EHR in real-time. Self-reporting of depression symptoms through these tools has been shown to reduce stigma and encourage more accurate symptom disclosure.
Physicians could readily access self-reported depression measures within Epic, enabling efficient review of scores, updates to patient conditions, and medication management. VitalSign6 provided a diagnostic checklist and decision support tools to guide the development of personalized treatment plans. Treatment options included pharmacological interventions utilizing MBC principles, behavioral therapies such as psychotherapy (integrated within the clinic), exercise regimens, symptom monitoring, specialist referrals, or no further follow-up. The system also facilitated scheduling follow-up appointments within 4 to 6 weeks to monitor patient progress.
Follow-up Visit Protocol
During follow-up visits, patients completed the PHQ-9 and other relevant measures during check-in. Based on patient self-reports and physician clinical assessments, decision support tools within VitalSign6 aided in determining whether to continue, modify, or escalate treatment, schedule further follow-up, or refer to specialists. The MBC program provided physicians with a systematic framework for managing, treating, and referring patients based on their symptom responses.
Provider and Staff Satisfaction Assessment
Provider and staff satisfaction with depression care and the VitalSign6 system were assessed using a Likert-type scale survey, administered before and after project implementation. Surveys explored knowledge of depression, comfort levels in discussing depression with patients, preferred settings for depression care, and perceptions of VitalSign6’s value. Mann-Whitney U tests were used to analyze paired Likert-type scale items. Post-survey, open-ended questions gathered qualitative feedback on the most challenging and valuable aspects of VitalSign6. Thematic analysis was used to identify recurring themes from written responses.
Outcome Measures and Analysis
Outcome measures were defined using the SMART (Specific, Measurable, Achievable, Relevant, Time-Bound) framework. Program fidelity was assessed using descriptive statistics, measuring screening rates, positive screening rates, and MBC administration rates. Clinical outcomes were evaluated by analyzing changes in patient-reported PHQ-9 scores from baseline to follow-up using paired t tests. Process outcomes focused on physician and staff satisfaction and beliefs, analyzed using Mann-Whitney U tests on paired Likert-type scale items. Data were collected from the EHR and UTSW’s REDCap database, and statistical analyses were performed using IBM SPSS v.25 with an alpha level of .05.
Results: Enhanced Screening and Improved Patient Outcomes with Depression Tools
Sample and Screening Rates
Between February and May 2019, 1200 unique adult patients were seen at the clinic. A high screening rate was achieved, with 95.4% (n=1145) of patients screened using the PHQ-2. Of those screened, 18.2% (n=208) screened positive based on PHQ-2 scores. Among PHQ-2 positive patients, 89.4% (n=186) were further screened using the PHQ-9. Technical issues impacted data recording for a small percentage (10.5%) of patients with positive PHQ-2 screens.
Notably, a significant proportion of patients (18.6%, n=214) with negative PHQ-2 screens but a history of depression or antidepressant medication were also screened with PHQ-9 due to BPA alerts. Additionally, 7.1% (n=81) of patients with negative PHQ-2 scores and no prior history were screened with PHQ-9 at physician request.
In total, 481 patients underwent PHQ-9 screening, with 62.8% (n=302) screening positive (score >4). Of these, 89.4% (n=270) received a diagnosis of depressive disorder. Among diagnosed patients, 87.4% (n=236) initiated MBC with personalized treatment plans, while 10% (n=27) were referred to specialty care, and 2.6% (n=7) declined treatment.
Depression Follow-up and Treatment Approaches
Of the 236 patients who commenced MBC, the majority (59.7%, n=141) received pharmacological treatment, 8.1% (n=19) received non-pharmacological interventions, and 31.3% (n=74) were recommended for symptom monitoring and rescreening. Patients were followed for 14 weeks post-diagnosis. A CONSORT flow diagram (Figure 2) illustrates patient progression through treatment and follow-up.
Figure 2. CONSORT Flow Diagram of Patient Progress Through Depression Treatment and Follow-up
Figure 2. CONSORT (Consolidated Standards of Reporting Trials) flow diagram. This diagram visually represents the flow of patients through the depression screening and treatment process, detailing enrollment, screening outcomes, diagnosis, treatment allocation, and follow-up completion.
Improvement in Depression Scores at Follow-up
Paired t-tests on 65 patients with complete data demonstrated a statistically significant reduction in self-reported PHQ-9 scores from baseline to follow-up (Figure 3). Mean PHQ-9 scores decreased from 14.89 at baseline to 9.58 at follow-up. Notably, 23.1% (n=15/65) of these patients achieved remission, defined as a PHQ-9 score <5, by the follow-up assessment.
Figure 3. Comparison of PHQ-9 Scores at Baseline and Follow-up
Figure 3. The 9-item Patient Health Questionnaire (PHQ-9) self-reported scores at baseline and follow-up. This graph illustrates the statistically significant decrease in average PHQ-9 scores from baseline to follow-up, indicating an improvement in patient-reported depression symptoms following the implementation of VitalSign6 and measurement-based care.
Physician and Staff Satisfaction with Depression Tools and VitalSign6
Physician Survey Results
Physician surveys revealed a statistically significant decrease in perceived importance of depression screening and MBC post-implementation, contrary to expectations. While pre-implementation median scores for the importance of screening and MBC were high (5 out of 5), post-implementation scores decreased to 4 (p=.002). Other survey items did not show statistically significant changes (Table 1).
Table 1. Physician Survey Results: Perceptions of Depression Care and VitalSign6
| Provider survey items | Pre-implementation Median (Min, Max) | Post-implementation Median (Min, Max) | P Value |
|---|---|---|---|
| How frequently are you currently treating depression? | 4.5 (3, 5) | 4 (3, 5) | .466 |
| My current understanding of depression is: | 4 (3, 5) | 4.5 (3, 5) | .912 |
| Depression is a chronic medical illness. | 5 (3, 5) | 4.5 (3, 5) | .217 |
| Depression in primary care patients is common. | 5 (4, 5) | 5 (4, 5) | .287 |
| Depression should mostly be treated by psychiatrists. | 1 (1, 5) | 2 (1, 3) | .494 |
| Primary care is the best setting to screen for depression. | 5 (3, 5) | 4 (3, 5) | .051 |
| When treating depression, it is important to use measures to assess symptoms. | 5 (4, 5) | 4 (3, 5) | .002 |
| I believe that it is important to screen patients for depression in my clinic. | 5 (4, 5) | 4 (4, 5) | .002 |
| I can accurately diagnose patients who screen positive for depression. | 4 (3, 5) | 4 (4, 5) | .328 |
| I am very familiar with how to use antidepressant medications. | 4 (2, 5) | 4 (1, 5) | .471 |
| I feel confident in knowing when to change antidepressant medications. | 4 (2, 5) | 4 (1, 4) | .270 |
| I know what medications can be used to augment an antidepressant medication. | 4 (2, 5) | 4 (1, 4) | .562 |
| I feel comfortable talking with my patients about their mental health. | 5 (3, 5) | 4.5 (4, 5) | .474 |
| How easy is the VitalSign6 software program to use with your daily workflow? | na | 2.5 (1,4) | nc |
| How easy is the VitalSign6 software program to use in the presence of patients? | na | 2.5 (1, 4) | nc |
| Overall, how easy is the VitalSign6 software program to use? | na | 3 (2, 4) | nc |
| How useful is the VitalSign6 software program in following a patient’s status over time? | na | 3.5 (1, 4) | nc |
| How useful do you find the treatment recommendations (clinical decision support) provided by the VitalSign6 software program? | na | 1.5 (1, 4) | nc |
| Overall, how useful is the VitalSign6 software program? | na | 3 (1, 4) | nc |
| How often does the VS6 software program draw your attention to issues or problems the patient is having that need to be addressed? | na | 3.5 (2, 5) | nc |
| To what extent has the VitalSign6program as a whole improved the quality of patient care that you are able to provide? | na | 3 (1, 4) | nc |
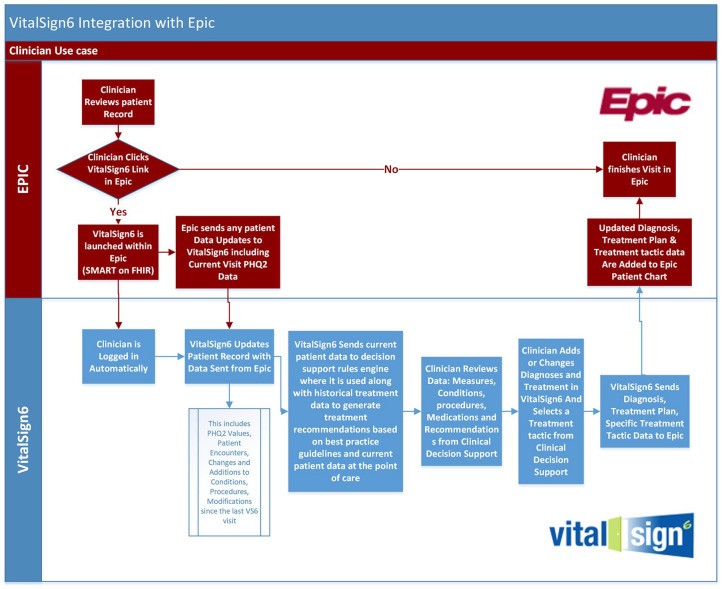
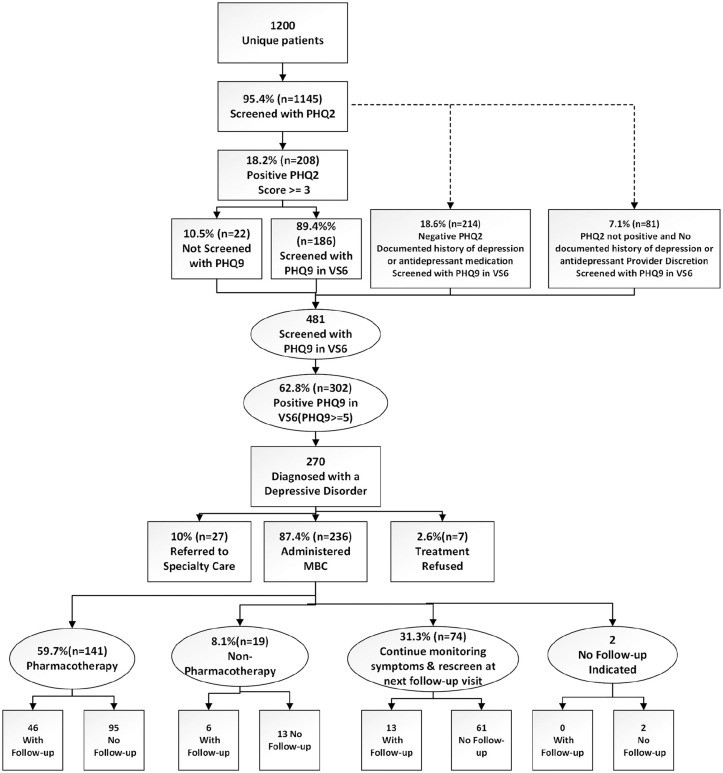
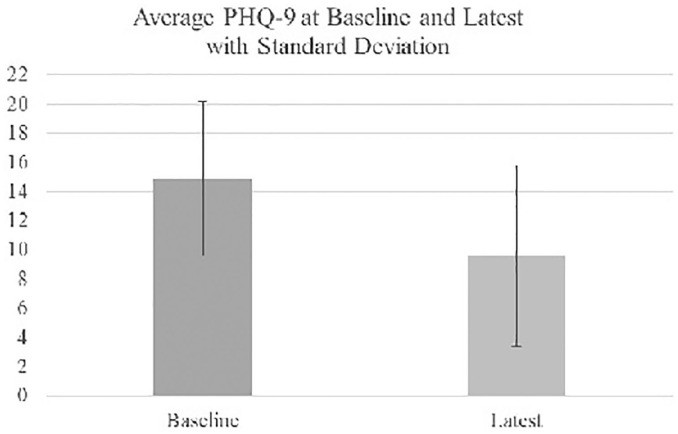
Table 1. Provider Survey Results. This table presents the median responses and ranges for physician survey items before and after the implementation of VitalSign6, along with p-values indicating the statistical significance of changes. Note the statistically significant decrease in perceived importance of depression screening and MBC post-implementation.
Staff Survey Responses
Staff surveys showed a statistically significant increase in staff comfort levels discussing mental health with patients post-implementation (p=.044). Other survey items did not reveal significant changes (Table 2).
Table 2. Staff Survey Results: Perceptions of Depression Care and VitalSign6
| Staff survey items | Pre-implementation Median (Min, Max) | Post-implementation Median (Min, Max) | P Value |
|---|---|---|---|
| My current understanding of depression is: | 3 (3, 5) | 4 (3, 5) | .362 |
| Depression is a chronic medical illness. | 4 (3, 5) | 4.5 (2, 5) | .935 |
| Depression in primary care patients is common. | 4 (3, 5) | 4 (4, 5) | .622 |
| Depression should mostly be treated by psychiatrists. | 3 (2, 5) | 2 (1, 5) | .057 |
| Primary care is the best setting to screen for depression. | 4 (2, 5) | 4.5 (3, 5) | .080 |
| I believe that it is important to screen patients for depression in my clinic. | 4 (3, 5) | 4.5 (3, 5) | .083 |
| I feel comfortable talking with my patients about their mental health. | 3 (1, 4) | 4 (1, 5) | .044 |
| How easy is the VitalSign6 software program to use with your daily workflow? | — | 2.5 (1, 5) | — |
| Overall, how easy is the VitalSign6 software program to use? | — | 3 (2, 5) | — |
| Overall, patients are receptive to depression screening using the VitalSign6 software program. | — | 2 (1, 4) | — |
| To what extent does your role contribute to patients receiving quality care for depression? | — | 3.5 (2, 5) | — |
Table 2. Staff Survey Results. This table summarizes the median responses and ranges for staff survey items before and after VitalSign6 implementation, along with p-values indicating statistical significance. Note the statistically significant increase in staff comfort levels discussing mental health with patients post-implementation.
Qualitative Feedback from Open-Ended Survey Questions
Qualitative analysis of open-ended survey responses revealed workflow disruption and technical interoperability issues as primary challenges with VitalSign6, reported by both physicians and staff. Physicians also expressed a desire for more robust decision support tools. Conversely, EHR integration, improved screening, and heightened mental health awareness were identified as the most valuable aspects of VitalSign6 by both groups. On-site support from the VitalSign6 team was also valued by staff.
Discussion: Impact of Depression Tools and MBC on Primary Care
This quality improvement project demonstrated the effectiveness of implementing depression screening tools and measurement-based care (MBC) in a primary care setting. Patient remission rates significantly improved from 0% to 23.1% post-intervention. This improvement is attributed to the combined effect of systematic screening, diagnosis, and MBC-driven treatment utilizing evidence-based CDS tools integrated with the EHR. The findings underscore the potential of EHR-integrated CDS systems to enhance depression screening and remission rates in primary care.
Both physicians and staff recognized the positive impact of VitalSign6 on mental health awareness and depression screening within the clinic. The two-step screening process using PHQ-2 and PHQ-9, facilitated by real-time EHR integration, proved effective in increasing screening rates to over 95%. The high diagnostic yield (89% of PHQ-9 positive patients diagnosed with depression) further highlights the utility of these depression tools in primary care. The established validity, reliability, and brevity of PHQ-2 and PHQ-9 support their use as preferred screening instruments in this setting. The clinic’s prior participation in the Delivery System Reform Incentive Payment (DSRIP) program, which incentivized depression screening, may have also contributed to the high baseline screening rate.
The study’s findings support the concept of managing depression as a triageable condition within primary care, rather than solely a mental health access issue. VitalSign6 equipped providers with evidence-based tools and CDS, enabling them to effectively manage 87.4% of diagnosed patients within primary care, with only 10% requiring specialist referral. This approach, incorporating pharmacological and non-pharmacological treatments, aligns with collaborative care models and reinforces the primary care physician’s clinical judgment. The results are consistent with previous studies demonstrating the effectiveness of VitalSign6 in diverse primary care settings.
The unexpected decrease in physician-perceived importance of depression screening and MBC post-implementation is likely related to workflow disruptions and technical challenges encountered during the project. Workflow integration and interoperability issues were the most frequently cited concerns in qualitative feedback. The simultaneous implementation of Epic Welcome tablets and VitalSign6 into existing clinic workflows created an initial learning curve. Ongoing EHR system upgrades are expected to address some of these interoperability challenges and further streamline VitalSign6 integration.
The significant improvement in staff comfort discussing mental health with patients highlights the positive impact of training and on-site support provided during project implementation. This suggests that targeted educational initiatives can effectively enhance staff capacity to address mental health concerns within primary care settings.
Limitations
The study’s limitations include its single-site design within an academic medical center residency program, which may limit generalizability. The project focused primarily on PHQ-2 and PHQ-9 measures and did not fully utilize the broader range of assessment tools available within VitalSign6, such as measures for anxiety, treatment side effects, and adherence. Furthermore, a high patient attrition rate (70.2% not returning for follow-up) warrants further investigation into factors influencing retention and strategies to improve follow-up rates, such as care coordination, patient engagement interventions, and teletherapy.
Conclusion: Enhancing Depression Care in Primary Care with Effective Tools
This implementation project demonstrates the value of integrating evidence-based depression tools and measurement-based care into primary care settings. VitalSign6 provided primary care physicians with essential tools for depression identification, treatment, and referral management, leading to improved patient outcomes and enhanced screening rates. Future efforts should focus on refining integrated care models, streamlining workflows, optimizing reporting mechanisms, and establishing sustainable implementation policies. These findings contribute to the growing evidence base supporting VitalSign6 as an effective tool for improving depression care within primary care and highlight the broader potential of depression tools and MBC to transform mental health service delivery in these settings.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Kimberly A. Siniscalchi https://orcid.org/0000-0002-7129-0821